Stem cell findings may offer answers for some bladder defects and disease

The breakthrough, developed at the UC Davis Institute for Regenerative Cures and published today in the scientific journal Stem Cells Translational Medicine, is significant because it provides a pathway to regenerate replacement bladder tissue for patients whose bladders are too small or do not function properly, such as children with spina bifida and adults with spinal cord injuries or bladder cancer.
“Our goal is to use human stem cells to regenerate tissue in the lab that can be transplanted into patients to augment or replace their malfunctioning bladders,” said Eric Kurzrock, professor and chief of the division of pediatric urologic surgery at UC Davis Children's Hospital and lead scientist of the study, which is titled “Induction of Human Embryonic and Induced Pluripotent Stem Cells into Urothelium.”
To develop the bladder cells, Kurzrock and his UC Davis colleagues investigated two categories of human stem cells. In their key experiments, they used induced pluripotent stem cells (iPS cells), which were derived from lab cultures of human skin cells and umbilical blood cells that had been genetically reprogrammed to convert to an embryonic stem cell-like state.
If additional research demonstrates that grafts of bladder tissue grown from human stem cells will be safe and effective for patient care, Kurzrock said that the source of the grafts would be iPS cells derived from a patient’s own skin or umbilical cord blood cells. This type of tissue would be optimal, he said, because it lowers the risk of immunological rejection that typifies most transplants.
In their investigation, Kurzrock and his colleagues developed a protocol to prod the pluripotent cells into becoming bladder cells. Their procedure was efficient and, most importantly, the cells proliferated over a long period of time – a critical element in any tissue engineering application.
“What’s exciting about this discovery is that it also opens up an array of opportunities using pluripotent cells,” said Jan Nolta, professor and director of the UC Davis Stem Cell program and a co-author on the new study. “When we can reliably direct and differentiate pluripotent stem cells, we have more options to develop new and effective regenerative medicine therapies. The protocols we used to create bladder tissue also provide insight into other types of tissue regeneration.”
UC Davis researchers first used human embryonic stem cells obtained from the National Institutes of Health’s repository of human stem cells. Embryonic stem cells can become any cell type in the body (i.e., they are pluripotent), and the team successfully coaxed these embryonic stem cells into bladder cells. They then used the same protocol to coax iPS cells made from skin and umbilical cord blood into bladder cells, called urothelium, that line the inside of the bladder. The cells expressed a very unique protein and marker of bladder cells called uroplakin, which makes the bladder impermeable to toxins in the urine.
The UC Davis researchers adjusted the culture system in which the stem cells were developing to encourage the cells to proliferate, differentiate and express the bladder protein without depending upon signals from other human cells, said Kurzrock. In future research, Kurzrock and his colleagues plan to modify the laboratory cultures so that they will not need animal and human products, which will allow use of the cells in patients.
Kurzrock’s primary focus as a physician is with children suffering from spina bifida and other pediatric congenital disorders. Currently, when he surgically reconstructs a child’s defective bladder, he must use a segment of their own intestine. Because the function of intestine, which absorbs food, is almost the opposite of bladder, bladder reconstruction with intestinal tissue may lead to serious complications, including urinary stone formation, electrolyte abnormalities and cancer. Developing a stem cell alternative not only will be less invasive, but should prove to be more effective, too, he said.
Another benefit of the UC Davis study is the insight it may provide about the pathways of bladder cancer, which is diagnosed in more than 70,000 Americans each year, according to the National Cancer Institute. “Our study may provide important data for basic research in determining the deviations from normal biological processes that trigger malignancies in developing bladder cells,” said Nolta. More than 90 percent of patients who need replacement bladder tissue are adults with bladder cancer. Kurzrock said “cells from these patients’ bladders cannot be used to generate tissue grafts because the implanted tissue could carry a high risk of becoming cancerous. On the other hand, using bladder cells derived from patients’ skin may alleviate that risk. Our next experiments will seek to prove that these cells are safer.”
The UC Davis research was supported by a grant from the California Institute for Regenerative Medicine (the state stem cell agency). Shriner’s Hospitals for Children has also provided Dr. Kurzrock with grant funds to explore pediatric bladder tissue regeneration.
In addition to Kurzrock and Nolta, co-authors of the paper are Stephanie L. Osborn, Ravikumar Thangappan, Ayala Luria, and Justin H. Lee.
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
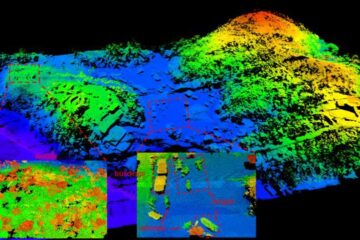
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















