Hopkins researchers discover how nitric oxide prevents blood vessel inflammation

Johns Hopkins scientists investigating nitric oxide (NO) – the molecular messenger that contributes to body functions as wide-ranging as cell death, new blood vessel growth and erections – have figured out how it can block blood vessel inflammation and prevent clotting, a process that has long stumped biologists.
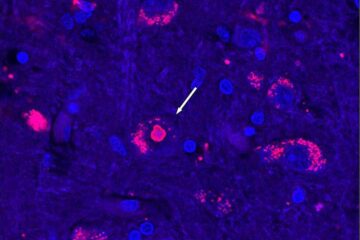
Reporting in the Oct. 17 issue of the journal Cell, cardiologist Charles J. Lowenstein, M.D., and his team observed that NO has the power to inhibit endothelial cells lining blood vessels from releasing inflammatory substances.
Normally, these cells activate a process called exocytosis (a release of substances) to start inflammation, releasing packets of molecules into the bloodstream that, like tiny hand grenades, explode and discharge compounds that trigger inflammation. NO can move in and target a protein within the endothelial cells, N-ethylmaleimide-Sensitive Factor (NSF), that stops the process from happening by blocking the ability of NSF to push out the molecules.
“Nitric oxide may regulate exocytosis this way in a variety of diseases,” says Lowenstein, an associate professor of medicine at Hopkins. “For example, nitric oxide blocks exocytosis from platelets, preventing blood clots; exocytosis from neurons, decreasing neurotoxicity in strokes; and exocystosis from lymphocytes, reducing autoimmune damage.”
The Hopkins scientists discovered NO’s protective role in both cells and mice. They added NO to human endothelial cells in culture and discovered that it blocked the release of inflammatory compounds. The researchers then found that platelets stuck to blood vessels more often in mice that could not make NO, compared to normal mice.
The findings already have led Lowenstein’s team to develop a novel drug to block exocytosis, thereby acting as an anti-clotting agent. It is a peptide that blocks exocytosis by a mechanism similar to that of nitric oxide. In laboratory tests in mice, the drug prevented tiny, disk-shaped platelets from sticking and causing blood clots. The therapy has potential to limit the amount of heart muscle damage following heart attack, or to treat people with blood-clotting disorders, Lowenstein says, but clinical trials are still years away.
The study was funded by the National Institutes of Health, the American Heart Association, Hopkins’ Ciccarone Center for the Prevention of Heart Disease, and the John and Cora H. Davis Foundation.
Coauthors were Kenji Matsushita, Craig N. Morrell, Shui-Xiang Yang, Munekazu Yamakuchi, Clare Bao, Makoto Hara, Richard A. Quick, Wangsen Cao, Brian O’Rourke and Jonathan Pevsner of Hopkins; Beatrice Cambien and Denisa D. Wagner of Harvard Medical School, and John M. Lowenstein of Brandeis University.
Matsushita, K. et al, “Nitric Oxide Regulates Exocytosis by S-Nitrosylation of N-ethylmaleimide-Sensitive Factor,” Cell, Oct. 17, 2003, Vol. 115, pages 1-20.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Recovering phosphorus from sewage sludge ash
Chemical and heat treatment of sewage sludge can recover phosphorus in a process that could help address the problem of diminishing supplies of phosphorus ores. Valuable supplies of phosphorus could…

Efficient, sustainable and cost-effective hybrid energy storage system for modern power grids
EU project HyFlow: Over three years of research, the consortium of the EU project HyFlow has successfully developed a highly efficient, sustainable, and cost-effective hybrid energy storage system (HESS) that…
After 25 years, researchers uncover genetic cause of rare neurological disease
Some families call it a trial of faith. Others just call it a curse. The progressive neurological disease known as spinocerebellar ataxia 4 (SCA4) is a rare condition, but its…





















