Chili peppers and inflammation: Researchers unravel mechanism of pain sensitivity

Scientists at Massachusetts General Hospital (MGH) have discovered a common component to the burning sensation produced by chili peppers and the pain associated with arthritis. The finding, published in the September 26 issue of Neuron, could help scientists devise new strategies to block the pain hypersensitivity associated with inflammation.
“The receptor activated by chili peppers in the mouth and other tissues also increases in the terminals of sensory neurons in the skin after inflammation, and this contributes to pain hypersensitivity,” says Clifford Woolf, MD, PhD, director of the Neural Plasticity Research Group in the Department of Anesthesia and Critical Care at MGH. A receptor is a protein that transports a chemical signal into a cell.
Woolf and lead author Ru-Rong Ji, PhD, also of the MGH Neural Plasticity Research Group, found that the increased production of the receptor following inflammation is mediated by a signal molecule called p38, located within sensory neurons. The chili pepper receptor, which is technically called TRPV1, responds to capsaicin, the chemical that is responsible for the “hot” in peppers. It also responds to actual heat and to low pH, a condition that occurs with inflammation.
“With these findings, we’re starting to understand why patients with arthritis or other inflammatory conditions are likely to have increased pain and sensitivity to heat,” says Woolf. He and his research team were surprised to find that the activation of p38 can cause a twenty-fold increase in the amount of TRPV1 protein in the skin but not in the activity of the gene coding for TRPV1.
“This means that the chili pepper receptor is not being regulated by the gene being switched on but by more protein being produced, an unexpected form of regulation,” says Ji. He also notes that their findings will open up new options for pain management. “We could use an inhibitor to p38 to block the increase in TRPV1, therefore blocking pain in patients who suffer from many diseases and conditions that involve inflammation.”
Following inflammation, the activation of p38 is very precise. The scientists found that it is caused by a specific growth factor signal acting on a particular subset of pain sensory neurons. There are a variety of pain sensations that create different changes within neurons, and all of the signals that are generated have not yet been identified. Each new discovery, like the current finding by the MGH researchers, sheds light on these complex pathways and brings new treatment strategies closer.
Media Contact
More Information:
http://www.mgh.harvard.edu/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
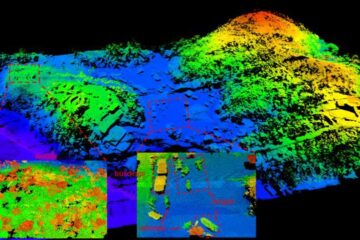
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















