New way to generate abundant functional blood vessel cells from human stem cells discovered

In a significant step toward restoring healthy blood circulation to treat a variety of diseases, a team of scientists at Weill Cornell Medical College has developed a new technique and described a novel mechanism for turning human embryonic and pluripotent stem cells into plentiful, functional endothelial cells, which are critical to the formation of blood vessels.
Endothelial cells form the interior “lining” of all blood vessels and are the main component of capillaries, the smallest and most abundant vessels. In the near future, the researchers believe, it will be possible to inject these cells into humans to heal damaged organs and tissues.
The new approach allows scientists to generate virtually unlimited quantities of durable endothelial cells — more than 40-fold the quantity possible with previous approaches. Based on insights into the genetic mechanisms that regulate how embryonic stem cells form vascular endothelial cells, the approach may also yield new ways to study genetically inherited vascular diseases. The study appears in the advance online issue of Nature Biotechnology.
“This technique is the first of its kind with serious potential as a treatment for a diverse array of diseases, especially cardiovascular disease, stroke and vascular complications of diabetes,” says Dr. Shahin Rafii, the study's senior author. Dr. Rafii is the Arthur B. Belfer Professor in Genetic Medicine and co-director of the Ansary Stem Cell Institute at Weill Cornell Medical College, and an investigator of the Howard Hughes Medical Institute.
In recent years, enormous hopes have been pinned on stem cells as the source of future cures and treatments. Indeed, human embryonic stem cells have the potential to become any one of the more than 200 types of adult cells. However, the factors and pathways that govern their differentiation to abundant derivatives that could be used to repair organs have remained poorly understood.
A major challenge for Dr. Rafii's lab has been to improve their understanding, and hence control, of the differentiation process (how stem cells convert to various cell types), and then to generate enough vascular endothelial cells — many millions — so they can be used therapeutically.
To meet this challenge, the scientists first screened for molecular factors that come into play when stem cells turn into endothelial cells. Their findings led them to a strategy that significantly boosts the efficiency of producing these cells.
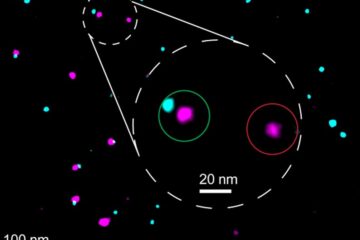
Then, the researchers tracked the differentiation process in real-time using a green fluorescent protein marker developed by Dr. Daylon James, the study's first author and assistant research professor in the Department of Reproductive of Medicine at Weill Cornell Medical College. They found that when they exposed stem cells to a compound that blocks TGF-beta (a growth factor involved in cell specialization) at just the right time during cell culturing, the propagation of endothelial cells dramatically increased.
Even more striking, they found that the cells worked properly when injected into mice. The cells were quickly assimilated into the animals' circulatory systems, and functioned alongside normal vasculature.
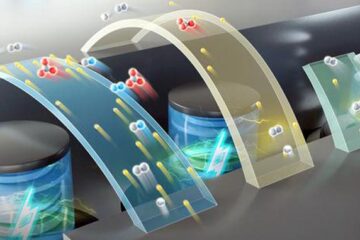
To achieve long-lasting clinical benefits, there remain additional hurdles to exploiting endothelial cells generated in vitro. Indeed, a fundamental prerequisite to using vascular cells in regenerative medicine has been the proper assembly in vivo of new blood vessels from stem-cell-derived cells, according to Dr. Sina Rabbany, who is an adjunct professor at Weill Cornell Medical College and professor of bioengineering at Hofstra University. Dr. Rabbany emphasizes that, in addition to manipulating biological factors implicated in endothelial cell differentiation, the impact of blood flow on endothelial cells is critical to engineering durable, vascularized organs. With the plentiful supply of endothelial cells that the new methods provide, Dr. Rabbany's team is working to build biological scaffolds that model the microenvironment of the vasculature, so that the vessels they generate will be functional and long-lasting in patients.
Another major obstacle to clinical use of cultured endothelial cells is the potential of immune rejection when the cells are injected into a patient. To address this risk, one approach would be to create a large, genetically diverse bank of human embryonic stem cells that, on demand, could be converted into endothelial cells that are compatible with specific patients.
“Given the success rate our group has shown in generating human embryonic stem cells from donated normal and diseased embryos, this new approach has broad implications not only for regenerative medicine, but also for the study of genetic diseases of the vasculature,” states Dr. Zev Rosenwaks, who is director and physician-in-chief of the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine as well as the director of the Tri-Institutional Stem Cell Initiative Derivation Unit at Weill Cornell Medical College.
The new endothelial cell culture is currently being validated in ongoing research at Weill Cornell using a number of stem cell “lines,” or “families” of stem cells. “Employing a highly sophisticated derivation technology, we have been able to generate 11 normal and diseased human embryonic cell lines from discarded embryos at the Tri-Institute Derivation Unit at Weill Cornell,” states Dr. Nikica Zaninovic, an assistant professor at the Department of Reproductive of Medicine who is spearheading the human embryonic stem cell derivation effort. Using the new differentiation methods, several of these new embryonic stem cell lines have been turned into vascular cells.
Testing in humans is the next major step in verifying the ability of this breakthrough cell-based approach to restore blood supply to injured organs. Armed with this new technology and under the umbrella of support from the Ansary Stem Cell Institute and Tri-Institutional Stem Cell Initiative (Tri-SCI), this team of scientists is hoping to transfer their methods to the clinic within the next five years.
The current study sheds light on the generation of human embryonic vasculature in ways that have not previously been feasible due to obstacles associated with the use of human embryonic tissue. As Dr. James explains, “The unbiased screening technique we used is a major technological advance that opens up possibilities for discovery of how human embryonic stem cells morph into the specific mature cells that compose the brain, liver, pancreas, and so on. Our general approach can be applied to additional human tissues and help other stem cell research groups develop and maintain specialized cell types in the larger effort to understand human development — and to heal many different kinds of human diseases and injuries.”
The Tri-Institutional Stem Cell Initiative, supported by a generous gift from The Starr Foundation, is a collaborative venture of Memorial Sloan-Kettering Cancer Center, The Rockefeller University, and Weill Cornell Medical College.
Ansary Stem Cell Institute
The Ansary Stem Cell Institute, established at Weill Cornell Medical College in 2004 through the generous donation of Shahla and Hushang Ansary, brings together a premier team of scientists to focus on stem cells — the primitive, unspecialized cells with an unrivaled capacity to form all types of cells, tissues and organs in the body. The vision of the Ansary Institute is to help lead the way in 21st-century medicine by employing this new field of research with tremendous potential to relieve human suffering. The Institute permits the multidisciplinary collaboration and creativity of Weill Cornell's researchers, as well as helps to attract the best and brightest young researchers in the field. Scientists at the Institute hope to discover the wellspring of adult stem cells in the body and ways to manipulate them to treat human illness. In particular, they hope to understand the regulation of cells that give rise to such essential components as blood vessels, insulin-producing cells in the pancreas (which are damaged in diabetics), and neurons of the brain and nervous system.
Weill Cornell Medical College
Weill Cornell Medical College, Cornell University's medical school located in New York City, is committed to excellence in research, teaching, patient care and the advancement of the art and science of medicine, locally, nationally and globally. Physicians and scientists of Weill Cornell Medical College are engaged in cutting-edge research from bench to bedside, aimed at unlocking mysteries of the human body in health and sickness and toward developing new treatments and prevention strategies. In its commitment to global health and education, Weill Cornell has a strong presence in places such as Qatar, Tanzania, Haiti, Brazil, Austria and Turkey. Through the historic Weill Cornell Medical College in Qatar, the Medical College is the first in the U.S. to offer its M.D. degree overseas. Weill Cornell is the birthplace of many medical advances — including the development of the Pap test for cervical cancer, the synthesis of penicillin, the first successful embryo-biopsy pregnancy and birth in the U.S., the first clinical trial of gene therapy for Parkinson's disease, and most recently, the world's first successful use of deep brain stimulation to treat a minimally conscious brain-injured patient. Weill Cornell Medical College is affiliated with NewYork-Presbyterian Hospital, where its faculty provides comprehensive patient care at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. The Medical College is also affiliated with the Methodist Hospital in Houston, making Weill Cornell one of only two medical colleges in the country affiliated with two U.S.News & World Report Honor Roll hospitals.
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
High-energy-density aqueous battery based on halogen multi-electron transfer
Traditional non-aqueous lithium-ion batteries have a high energy density, but their safety is compromised due to the flammable organic electrolytes they utilize. Aqueous batteries use water as the solvent for…

First-ever combined heart pump and pig kidney transplant
…gives new hope to patient with terminal illness. Surgeons at NYU Langone Health performed the first-ever combined mechanical heart pump and gene-edited pig kidney transplant surgery in a 54-year-old woman…
Biophysics: Testing how well biomarkers work
LMU researchers have developed a method to determine how reliably target proteins can be labeled using super-resolution fluorescence microscopy. Modern microscopy techniques make it possible to examine the inner workings…





















