Loss of nerve cells may link constipation with achalasia of the oesophagus

Patients who have difficulty swallowing food may also be more likely to suffer from constipation, according to a preliminary study published this week in BMC Gastroenterology. The research suggests that patients with achalasia of the oesophagus, associated with a loss of nerve cells in the muscle surrounding the oesophagus, may also lose nerve cells from the muscle surrounding the rectum. This may cause an increased incidence of constipation in this population.
Patients who suffer from achalasia of the oesophagus have problems passing food from their oesophagus to their stomach. Normally when you swallow, food is passed down the oesophagus aided by waves of muscle contraction called peristalsis. The sphincter muscle at the base of the oesophagus opens to allow food to pass into the stomach and then closes to prevent the stomach acid from entering the oesophagus. Both peristalsis and the relaxation of the sphincter muscle are controlled by the autonomic nervous system. The loss of nerve cells in the muscle surrounding the oesophagus therefore inhibits both these processes, leading to a build up of food in the oesophagus, causing it to stretch.
As constipation is similarly characterised by the impeded passage of the contents of the lower intestine, Professor Ahmed Shafik, from Cairo University, was interested in studying the link between achalasia and constipation. He tested nine people with achalasia, and eight healthy volunteers for symptoms of constipation. Six of the nine patients with achalasia had constipation, while none of the control subjects did. The six patients with constipation showed a lack of nerve cells in the muscular tissue surrounding their rectum and they did not have a normal rectoanal inhibitory reflex.
Professor Shafik suggests that the loss of nerve cells caused the constipation in these patients. It seems unlikely to be a secondary effect of the achalasia itself, as constipation often preceded the inability to eat that is symptomatic of achalasia. Furthermore, when the achalasia was treated, the constipation remained.
Although the high incidences of constipation in patients with achalasia, as well as the loss of nerve cells in both conditions, suggest a relationship between the two, this study did not elucidate its nature. Further work is needed to find out why the nerve cells degenerate in these patients, and why this degeneration appears to happen only at the extremities of the gut. However, this research is an important guide for future studies.
Media Contact
More Information:
http://www.biomedcentral.com/1471-230X/3/27/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
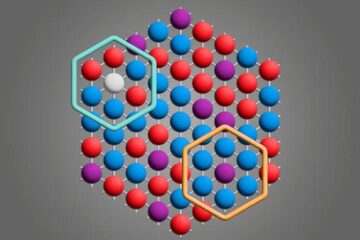
Microscopic basis of a new form of quantum magnetism
Not all magnets are the same. When we think of magnetism, we often think of magnets that stick to a refrigerator’s door. For these types of magnets, the electronic interactions…

An epigenome editing toolkit to dissect the mechanisms of gene regulation
A study from the Hackett group at EMBL Rome led to the development of a powerful epigenetic editing technology, which unlocks the ability to precisely program chromatin modifications. Understanding how…
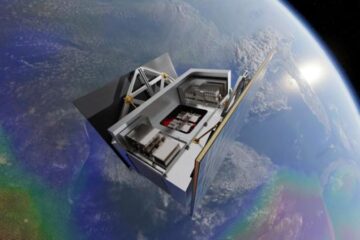
NASA selects UF mission to better track the Earth’s water and ice
NASA has selected a team of University of Florida aerospace engineers to pursue a groundbreaking $12 million mission aimed at improving the way we track changes in Earth’s structures, such…





















