Dry eye disease alters how the eye’s cornea heals itself after injury
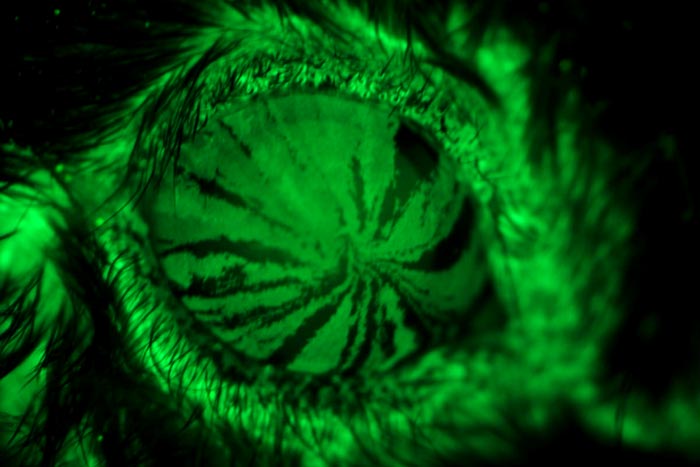
Studying mice, researchers at Washington University School of Medicine in St. Louis have found that proteins made by stem cells to help regenerate the cornea may become new targets for treating and preventing injuries to the cornea related to dry eye disease. When eyes are dry, the cornea is more susceptible to injury. By tracking the movements of stem cells (in fluorescent green) in a mouse eye, researchers were able to trace the cells as they differentiated into corneal cells and migrated to the center of the cornea, providing clues about how the cells work to help corneal injuries heal.
Credit: Washington University School of Medicine
Mouse study IDs gene and protein that could be targets for therapy.
People with a condition known as dry eye disease are more likely than those with healthy eyes to suffer injuries to their corneas. Studying mice, researchers at Washington University School of Medicine in St. Louis have found that proteins made by stem cells that regenerate the cornea may be new targets for treating and preventing such injuries.
The study is published online Jan. 2 in the Proceedings of the National Academy of Sciences.
Dry eye disease occurs when the eye can’t provide adequate lubrication with natural tears. People with the common disorder use various types of drops to replace missing natural tears and keep the eyes lubricated, but when eyes are dry, the cornea is more susceptible to injury.
“We have drugs, but they only work well in about 10% to 15% of patients,” said senior investigator Rajendra S. Apte, MD, PhD, the Paul A. Cibis Distinguished Professor in the John F. Hardesty, MD, Department of Ophthalmology & Visual Sciences. “In this study involving genes that are key to eye health, we identified potential targets for treatment that appear different in dry eyes than in healthy eyes. Tens of millions of people around the world — with an estimated 15 million in the United States alone — endure eye pain and blurred vision as a result of complications and injury associated with dry eye disease, and by targeting these proteins, we may be able to more successfully treat or even prevent those injuries.”
The researchers analyzed genes expressed by the cornea in several mouse models — not only of dry eye disease, but also of diabetes and other conditions. They found that in mice with dry eye disease, the cornea activated expression of the gene SPARC. They also found that higher levels of SPARC protein were associated with better healing.
“We conducted single-cell RNA sequencing to identify genes important to maintaining the health of the cornea, and we believe that a few of them, particularly SPARC, may provide potential therapeutic targets for treating dry eye disease and corneal injury,” said first author Joseph B. Lin, an MD/PhD student in Apte’s lab.
“These stem cells are important and resilient and a key reason corneal transplantation works so well,” Apte explained. “If the proteins we’ve identified don’t pan out as therapies to activate these cells in people with dry eye syndrome, we may even be able to transplant engineered limbal stem cells to prevent corneal injury in patients with dry eyes.”
Lin JB, Shen X, Pfeifer CW, Shiau F, Santeford A, Ruzycki PA, Clark BS, Liu Q, Huang AJW, Apte RS. Dry eye disease in mice activates adaptive corneal epithelial regeneration distinct from constitutive renewal in homeostasis. Proceedings of the National Academy of Sciences, Jan. 2, 2023.
The study was funded with support from the National Eye Institute, the National Institute of Diabetes and Digestive and Kidney Diseases and the National Institute of General Medical Sciences of the National Institutes of Health (NIH). Grant numbers: R01 EY019287, R01 EY027844, R01 EY024704, P30 EY02687, F30 DK130282, T32 GM07200 Additional funding provided by the Jeffrey T. Fort Innovation Fund, a Centene Corp. contract for the Washington University-Centene ARCH Personalized Medicine Initiative and Research to Prevent Blindness.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,700 faculty. Its National Institutes of Health (NIH) research funding portfolio is the fourth largest among U.S. medical schools, has grown 54% in the last five years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,790 faculty physicians practicing at over 60 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
DOI: 10.1073/pnas.2204134120
Method of Research: Experimental study
Subject of Research: Animals
Article Title: Dry eye disease in mice activates adaptive corneal epithelial regeneration distinct from constitutive renewal in homeostasi
Article Publication Date: 2-Jan-2023
Media Contact
Jim Dryden
Washington University School of Medicine
jdryden@wustl.edu
Office: 314-286-0110
Original Source
https://medicine.wustl.edu/?p=119177&preview=1&_ppp=3bd0b6479f
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
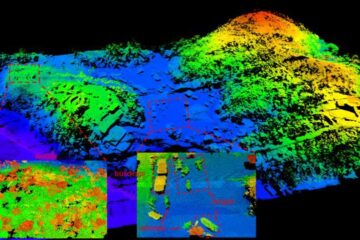
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















