Rethinking new therapies for Crohn’s disease at U.Va.

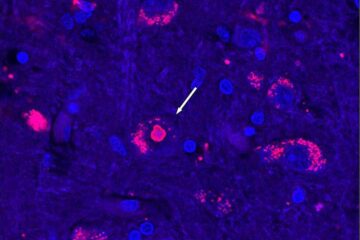
In a Perspective article in the Nov. 11 issue of the New England Journal of Medicine, Dr. Fabio Cominelli, chief of the division of gastroenterology and hepatology at the University of Virginia Health System reports that a dysregulated response by the innate immune system- the body’s initial, non-specific response to infection- may have more to do with the development of Crohn’s than acquired immunity, currently thought by many to be the most likely suspect.
Patients, physicians and medical researchers need to reconsider traditional hypotheses about the biological processes that underlie Crohn’s disease, according to Cominelli, a leading Crohn’s expert. More than half a million people in the U.S. suffer from Crohn’s,a chronic disease involving inflammation of the intestines.
Cominelli indicates that more cytokines- proteins that coordinate the immune response in inflammation- may be involved in Crohn’s than scientists had previously thought. He believes that a growing body of evidence shows that both type 1 and type 2 helper T-cells are likely involved in the early stages of Crohn’s disease. The classic paradigm held that cytokines secreted by type 1 T-cells, such as TNF (tumor necrosis factor), interleukin-12 and interferon-g were primarily responsible for Crohn’s, while type 2 cytokines were linked to ulcerative colitis, another type of inflammatory bowel disease.
Although the underlying cause of Crohn’s remains unclear, Cominelli describes an intriguing hypothesis in which a defective innate immune system may be an important player. This could mean that blocking specific type 1 cytokines in the initial phases of Crohn’s “may not be beneficial and could actually aggravate the existing disease process,” he writes.
Cominelli emphasizes that there are questions about infliximab, the first biological therapeutic approved to treat Crohn’s, which blocks the production of the type 1 cytokine TNF. He points out that infliximab therapy does not relieve Crohn’s symptoms or induce remission in some patients. Plus, type 1 cytokines are important in combating infections, and blocking them can reactivate latent tuberculosis in some patients.
Cominelli also warns that anti-cytokine therapy in general may increase the long-term risk of cancer, and blocking some cytokines may reactivate asthma. “An effective treatment strategy for such patients might involve the blockade of multiple cytokines in order to intervene in several pathways,” he concludes.
Media Contact
More Information:
http://www.virginia.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
After 25 years, researchers uncover genetic cause of rare neurological disease
Some families call it a trial of faith. Others just call it a curse. The progressive neurological disease known as spinocerebellar ataxia 4 (SCA4) is a rare condition, but its…
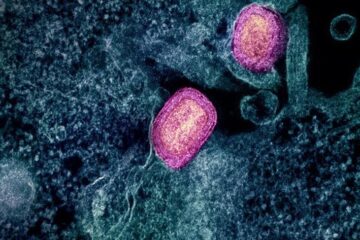
Lower dose of mpox vaccine is safe
… and generates six-week antibody response equivalent to standard regimen. Study highlights need for defined markers of mpox immunity to inform public health use. A dose-sparing intradermal mpox vaccination regimen…

Efficient, sustainable and cost-effective hybrid energy storage system for modern power grids
EU project HyFlow: Over three years of research, the consortium of the EU project HyFlow has successfully developed a highly efficient, sustainable, and cost-effective hybrid energy storage system (HESS) that…





















