Which drugs should health plans cover?

Five principles guide decisions that improve patient safety and lower costs, say Group Health experts
With the cost of prescription drugs rising faster than any other part of health care, more insurers and health systems have begun adopting restrictive policies for coverage of newer drugs. How can consumers and health care organizations be sure that such policies don’t lean too far in either direction–either restricting necessary treatment or wasting consumers’ premiums on expensive medicines that offer no real advantage?
These issues are addressed by experts from Group Health in an article in the October 2005 issue of the Journal of General Internal Medicine. The piece presents five principles that organizations can use to protect patients when they compare the benefits, risks, and costs of drugs to include in their “formularies,” the lists of drugs approved for coverage.
“Manufacturers of new drugs make a range of claims about clinical benefits, differences in cost, and cost effectiveness,” said Greg Simon, MD, MPH, a Group Health psychiatrist and researcher who is the lead author of the article. “Decision makers need some principles for sorting through those claims.” While other groups have established broad principles for addressing the problem, the Group Health authors offer “more specific rules for identifying the right questions and the most important evidence,” Simon explained.
In addition to Simon, co-authors on this paper include Bruce Psaty, MD, PhD, a Center for Health Studies senior investigator and University of Washington professor of medicine and epidemiology who is also a member of Institute of Medicine Committee on the Assessment of the U.S. Drug Safety System; Group Health physician Marc Mora, MD, former chair of the committee that establishes formulary policies for Group Health; and Group Health pharmacist Jennifer Berg Hrachovec, PharmD, MPH.
The five principles, described in more detail below, are:
1. Give more weight to true experiments than to models or simulations, and carefully examine assumptions of such models.
2. Give more weight to real health outcomes than changes in risk factors.
3. Look at the full range of alternatives rather than those selected by industry when considering claims for advantages of new treatments.
4. Understand that variation in effects across individuals or subgroups argues against restrictions on first-line treatment, but only if those differences are predictable.
5. Understand that variation in effects argues against requiring changes in ongoing treatment.
“The money we have available for health care is not unlimited,” said Simon. “Health insurers and government agencies that pay for health care have a responsibility to make sure the money we have is used for the greatest benefit. Our society tends to assume that a newer, more expensive treatment must be more effective. That assumption can be bad for our pocketbooks and our health.”
Principles for evidence-based drug formulary policy
1. Give more weight to true experiments than to models or simulations, and carefully examine assumptions of such models.
The highest standard for finding true differences between newer and older treatments is the “randomized controlled trial,” where study participants are assigned to different treatments by chance. Those “gold standard” comparisons are costly and may take years to complete. Policy makers sometimes rely on simulated comparisons, but those comparisons are often based on expert opinion and subject to bias. “When models or simulations are the best data available, appropriate skepticism is necessary,” the authors write.
As an example, they point to Cox-2 inhibitor drugs such as Vioxx and Celebrex, which are more expensive, but no more effective on average, than older anti-inflammatory drugs. Simulated comparisons supported by the pharmaceutical industry showed that Cox-2 inhibitors could save money in the long run by reducing the risk of ulcers and intestinal bleeding. But that claim was not consistently demonstrated in randomized comparisons. The most recent evidence now finds that Cox-2 inhibitors probably do not reduce intestinal side effects and probably do increase risk of heart problems.
“Fortunately, many health care organizations had weighed the true scientific evidence of the potential risks and benefits of these drugs and decided years ago not to include them in their formularies,” said Mora. “The principles we present can help organizations make these kinds of sound decisions in the interest of patient safety.”
2. Give more weight to real health outcomes than changes in risk factors.
Comparisons should give more credit to medications that are actually proven to result in less illness and fewer deaths, rather than simply changing risk factors. For example, many long-term medications, such as cholesterol or blood pressure drugs, are prescribed to reduce future risk of disease. While newer blood pressure drugs have been shown to reduce blood pressure, older and more affordable drugs are probably more effective for actually preventing heart disease, explained Simon.
3. Look at the full range of alternatives rather than those selected by industry when considering claims for advantages of new treatments.
Studies needed for new drug approval often compare a placebo with a current standard treatment. But sometimes there are many standard treatments available, and the manufacturer of a new drug may not always choose the most informative comparison. Psaty and his colleagues have developed a method called “network meta-analysis” that can be used to make valid comparisons across several treatments that are studied separately. This can be “especially important when the comparisons most interesting to clinicians and policy-makers differ from those that are most interesting or advantageous to research sponsors,” the authors write.
4. Understand that variation in effects across individuals or subgroups argues against restrictions on first-line treatment, but only if those differences are predictable.
Drugs approved for the same problem often show equal efficacy on average, but their effects can vary widely between individuals, the authors explain. “This …can be misinterpreted to support either unnecessarily broad or inappropriately restrictive formulary policies.” If it’s not possible to predict at the beginning of treatment which drug will have the best effect, then starting with the most affordable alternative makes sense, the authors contend. But a more expensive medication is often justified for patients who respond poorly to first-line treatment.
The authors use the class of drugs for depression known as serotonin reuptake inhibitors (SRIs) as an example. Direct randomized comparisons of SRIs show no difference in average effectiveness. But studies also show that half the patients who fail to respond to one SRI may do well on another. It’s not possible to predict who will do well on which drug at the beginning of treatment. Therefore, it makes sense for an insurance company to only cover the most affordable drug for anyone starting treatment for the first time, the authors write. Patients who do poorly with the first medication should be allowed to use one of the more expensive alternatives.
5. Understand that variation in effects argues against requiring changes in ongoing treatment.
With this principle, the authors argue that formulary changes should not necessarily result in requirements that patients switch to new drugs. “In addition to concern about variability in effect, decisions …must consider added visits and other costs of medication changes, as well as the likelihood that many physicians and patients may be hesitant to disrupt stable treatment,” the authors write.
About Group Health and the Center for Health Studies
Group Health is a consumer-governed, nonprofit health care system that coordinates care and coverage. Based in Seattle, Group Health and Group Health Options, Inc. serve nearly 550,000 members in Washington and Idaho. Group Health’s Center for Health Studies conducts research related to prevention, diagnosis, and treatment of major health problems. The Center for Health Studies is funded primarily through government and private research grants.
Media Contact
More Information:
http://www.ghc.orgAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
High-energy-density aqueous battery based on halogen multi-electron transfer
Traditional non-aqueous lithium-ion batteries have a high energy density, but their safety is compromised due to the flammable organic electrolytes they utilize. Aqueous batteries use water as the solvent for…

First-ever combined heart pump and pig kidney transplant
…gives new hope to patient with terminal illness. Surgeons at NYU Langone Health performed the first-ever combined mechanical heart pump and gene-edited pig kidney transplant surgery in a 54-year-old woman…
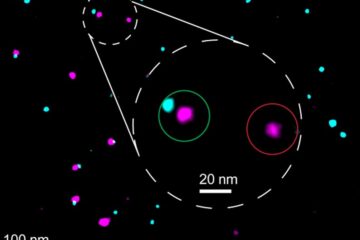
Biophysics: Testing how well biomarkers work
LMU researchers have developed a method to determine how reliably target proteins can be labeled using super-resolution fluorescence microscopy. Modern microscopy techniques make it possible to examine the inner workings…





















