Gene chips used to distinguish ventilator-associated pneumonia from underlying critical illness

Critically ill patients who need a ventilator to breathe face a high risk of pneumonia. The lung infection, however, is exceedingly difficult to diagnose because a patient's underlying condition often skews laboratory test results and masks pneumonia's symptoms – a reality that can delay appropriate antibiotic treatment.
Using gene chip technology, scientists at Washington University School of Medicine in St. Louis demonstrate for the first time they can distinguish pneumonia associated with ventilator use from other serious illnesses. The research, published Feb. 13 in the journal Public Library of Science One, suggests that the method may lead to early, more accurate detection and treatment of ventilator-associated pneumonia.
The team analyzed patterns of expression in more than 8,000 genes as patients on mechanical ventilators developed and recovered from pneumonia. They found changes in the activity of 85 genes could pinpoint early activation of the immune system in response to pneumonia, typically several days before clinical signs of the infection developed. By adding computational tools to their genomic analysis, the researchers also showed they could objectively monitor patients' recovery by graphing changes over time, creating a tool they called the “riboleukogram.”
“This is an important step toward the development of a specific molecular test for diagnosing infection – in particular pneumonia – and predicting patients' recovery,” says J. Perren Cobb, M.D., director of Washington University's Center for Critical Illness and Health Engineering and an intensivist at Barnes-Jewish Hospital. “If we could determine which patients are destined to develop pneumonia based on early changes in the activity of genes that regulate immune response, we could give them antibiotics sooner, with the hope that we might be able to prevent or curtail the infection.”
As one of the more common and deadly hospital-acquired infections, ventilator-associated pneumonia has recently become a target for both quality improvement and patient safety efforts. Up to 30 percent of patients on a ventilator develop pneumonia, statistics show, increasing length of stay and the risk of death while adding thousands of dollars to each patient's hospital bill. The breathing tube is inserted into patients' lungs, bypassing the body's natural protective mechanisms that normally filter out harmful bacteria. The air that is pumped through the tube also must be humidified, which creates a breeding ground for microorganisms.
Scientists have tried unsuccessfully for years to identify a single marker or a suite of markers that could diagnose infection in ICUs. While both fever and an elevated white blood cell count often indicate an infection in healthy individuals, the same symptoms are widespread in ICU patients, where they are linked to a range of underlying conditions, including trauma, shock, organ failure and surgical complications. Diagnosis of infection is even more complicated in patients on a ventilator because they are sedated and the breathing tube prevents them from talking.
The current study took Cobb and his Washington University colleagues from the laboratory bench to patients' bedsides as they refined their method to diagnose pneumonia. Initially, they used the gene chip technology in mice to identify 219 genes whose patterns of expression could distinguish pneumonia from widespread inflammation, another common condition in intensive care units that involves systemic activation of the immune system. The patterns of gene expression in mice also could differentiate between gram-negative bacteria (Pseudomonas), a common type responsible for ventilator-associated pneumonia, and gram-positive bacteria (Streptococcus), which is a frequent cause of pneumonia in a community setting.
The researchers then moved to the ICU to determine whether the activity of the equivalent human genes could differentiate between pneumonia and inflammation in patients breathing with the assistance of ventilators. They narrowed their focus to 11 of 20 patients who developed pneumonia more than two days after having a breathing tube inserted. These patients had blood samples drawn at 48-hour intervals to determine whether changes in gene expression could monitor patients' response to treatment and their recovery. Most of the patients developed pneumonia within three to six days of being on a ventilator. None of them died.
The researchers used microarray analysis to study gene expression patterns in infection-fighting white blood cells contained in the blood samples. They found alterations in the activity of 85 genes some 24 to 72 hours before diagnosis of pneumonia by the physician attending in the ICU.
“This suggests that we could start patients on antibiotics earlier, say at the first change in these genomic vital signs, and we likely could significantly improve their ability to recover from pneumonia,” Cobb says.
Many of the genes identified by the research team regulate specialized immune cells known as neutrophils. These cells dramatically increase in number as bacteria invade the body. “We found genes that control neutrophil activation were turned on, and that is consistent with someone developing a bacterial infection,” Cobb explains. “We did not find neutrophil genes being activated in patients who did not have infection, even though they had fevers and high white blood cell counts.”
Other genes of interest regulated messenger proteins called chemokines, which send signals recruiting immune cells to fight off infection.
The scientists confirmed the ability of their genomic analysis to diagnose infection and monitor recovery in a second small group of seven patients on mechanical ventilators, two of whom developed pneumonia. As the patients healed, alterations in the expression of the 85 genes diminished, indicating that they had returned to a healthy state.
“Dr. Cobb's work represents an important step forward in developing an objective way to diagnose ventilator associated-pneumonia in intensive care units and predict patients' recovery,” says Sarah Dunsmore, Ph.D., who oversees sepsis grants at the National Institute of General Medical Sciences, which partially funded the study. “This innovative approach has the potential to benefit patients, through earlier diagnosis and treatment, and to help hospitals better control outbreaks of pneumonia in patients on ventilator support.”
Cobb says he and his team now plan to evaluate the clinical usefulness of the genetic analysis in a larger, independent group of patients with ventilator-associated pneumonia.
Media Contact
More Information:
http://www.wustl.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
High-energy-density aqueous battery based on halogen multi-electron transfer
Traditional non-aqueous lithium-ion batteries have a high energy density, but their safety is compromised due to the flammable organic electrolytes they utilize. Aqueous batteries use water as the solvent for…

First-ever combined heart pump and pig kidney transplant
…gives new hope to patient with terminal illness. Surgeons at NYU Langone Health performed the first-ever combined mechanical heart pump and gene-edited pig kidney transplant surgery in a 54-year-old woman…
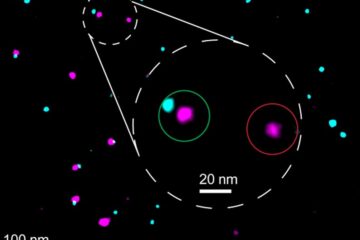
Biophysics: Testing how well biomarkers work
LMU researchers have developed a method to determine how reliably target proteins can be labeled using super-resolution fluorescence microscopy. Modern microscopy techniques make it possible to examine the inner workings…





















