Prostate cancer surgeons 'feel' with their eyes

Robotic surgical technology with its three-dimensional, high-definition view gives surgeons the sensation of touch, even as they operate from a remote console. A new study describes the phenomenon, called intersensory integration, and reports that surgical outcomes for prostate cancer surgery using minimally invasive robotic technology compare favorably with traditional invasive surgery.
Led by physician-scientists at NewYork-Presbyterian Hospital/Weill Cornell Medical Center and appearing in the March issue of British Journal of Urology International, the study is the first to show that a lack of tactile feedback during robotic surgery does not adversely impact outcomes in patients with prostate cancer. It also identified various visual cues that surgeons can use to improve clinical outcomes.
“Anatomical details and visual cues available through robotic surgery not only allow experienced surgeons to compensate for a lack of tactile feedback, but actually give the illusion of that sensation,” says Dr. Ashutosh Tewari, the study's lead author; professor of urology, urologic oncology, and public health at Weill Cornell Medical College; and director of the Lefrak Center of Robotic Surgery and the Institute of Prostate Cancer at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. “For patients, this means the safety of knowing the benefits of a robotic approach — including a quicker recovery — don't compromise the surgery's primary mission of removing the cancer.”
In recent years, robotic-assisted laparoscopic prostatectomy (RALP) has become a popular surgical method for treating prostate cancer because it is less invasive than traditional surgery. No studies have shown that RALP leads to worse outcomes, but doctors have wondered whether this was the case because surgeons often use their fingers to feel the prostate during traditional surgery to refine how much they cut to achieve the best outcome.
Cancer cells produce changes in tissue firmness that surgeons can sense. Because this tactile evaluation is not possible for surgeons using RALP, clinicians have wondered whether the robotic approach could lead surgeons to miss some cancer, and thus subject patients to a greater risk of cancer recurrence.
To find out, the investigators videotaped 1,340 RALPs. After every couple hundred procedures, they examined the pathology results of the prostate that was removed to determine the incidence of positive surgical margins, an indication that a surgeon might not have removed all of the cancer. In this study, the investigators focused on the posterolateral surgical margin (PLSM+), the area where the prostate is attached to the nerves.
“When you look at the entire specimen after surgery is done, you want to see cancer inside of the prostate but you don't want to see cancer touching the surface,” Dr. Tewari says. “After surgery we look at the specimen, and if there are no cancer cells touching the surface, we call that a negative margin. If cancer is touching the edge, then we say it has positive margins. This means there may be some cancer left in the patient.”
The investigators then studied the videotapes to determine what refinements in the procedure resulted in negative margins. Using this new knowledge to refine the surgery, they conducted the next couple hundred RALPs, reviewed the videotapes, refined their techniques, conducted the next round of RALPs, reviewed, refined and so on.
The investigators found that robotic surgery did not compromise outcomes. The incidence of PLSM+ was 2.1 percent, which gradually declined to 1 percent in the last 100 patients. Positive PLSMs are found in 2.8 percent to 9 percent of patients undergoing traditional prostatectomy.
The researchers say that the enhanced vision allowed by the robotic approach brings about a “reverse Braille phenomenon” or the ability to “feel” when vision is enhanced. They have identified a number of visual cues that clinicians can use to improve outcomes, including the color of tissue, the location of veins as a landmark for the location of nerves, signs of inflammation, and appreciation of so-called compartments outside the prostate.
Surgeons use a three-level approach to optimize outcomes in prostate surgery: the clinical exam including the prostate-specific antigen (PSA) test, magnetic resonance imaging (MRI) tests, and cues during the actual surgery itself. They use the clinical exam and MRI to determine which one of four types of nerve-sparing surgeries to conduct before the operation and then refine their technique during the actual procedure if cues indicate a need.
“Treat each patient individually, get as much as information from the clinical exam, biopsy, imaging, and learn to appreciate the anatomical changes,” Dr. Tewari says. “The outcomes of prostate cancer surgery are not just technology dependent, but rather they are dependent on surgical experience, anatomical details and attention to basic surgical techniques. Robotic surgery does not seem to compromise outcomes.”
“As someone with 30 years of experience as a pathologist, I, too, have developed the ability described in this paper. I can look at a tissue sample and know if it is firm or soft and what to expect in its pathology — something that helps me to home in on the area with the abnormality,” says Dr. Maria M. Shevchuk, the study's senior author, associate professor of pathology at Weill Cornell Medical College, and a pathologist at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. “It is only natural that this ability would also be present in experienced robotic surgeons.”
Co-authors of the study include Dr. Mohammed Akhtar, Dr. Youssef El-Douaihy, Robert A. Leung, Dr. Nishant D. Patel, Dr. E. Darracott Vaughan and Dr. Rajiv Yadav of NewYork-Presbyterian Hospital/Weill Cornell Medical Center; Drs. Muhul B. Amin, Mark A. Rubin and Jiangling J. Tu of Weill Cornell Medical College; Mark Burns and Usha Kreaden from Intuitive Surgical, Inc., Sunnyvale Calif.; and Dr. Atsushi Takenaka of Kobe University, Graduate School of Medicine, Kobe, Japan.
For more information, patients may call (866) NYP-NEWS.
NewYork-Presbyterian Hospital/Weill Cornell Medical Center
NewYork-Presbyterian Hospital/Weill Cornell Medical Center, located in New York City, is one of the leading academic medical centers in the world, comprising the teaching hospital NewYork-Presbyterian and Weill Cornell Medical College, the medical school of Cornell University. NewYork-Presbyterian/Weill Cornell provides state-of-the-art inpatient, ambulatory and preventive care in all areas of medicine, and is committed to excellence in patient care, education, research and community service. Weill Cornell physician-scientists have been responsible for many medical advances — including the development of the Pap test for cervical cancer; the synthesis of penicillin; the first successful embryo-biopsy pregnancy and birth in the U.S.; the first clinical trial for gene therapy for Parkinson's disease; the first indication of bone marrow's critical role in tumor growth; and, most recently, the world's first successful use of deep brain stimulation to treat a minimally conscious brain-injured patient. NewYork-Presbyterian Hospital also comprises NewYork-Presbyterian Hospital/Columbia University Medical Center, NewYork-Presbyterian Morgan Stanley Children's Hospital, NewYork-Presbyterian Hospital/Westchester Division and NewYork-Presbyterian Hospital/The Allen Hospital. NewYork-Presbyterian is the #1 hospital in the New York metropolitan area and is consistently ranked among the best academic medical institutions in the nation, according to U.S.News & World Report. Weill Cornell Medical College is the first U.S. medical college to offer a medical degree overseas and maintains a strong global presence in Austria, Brazil, Haiti, Tanzania, Turkey and Qatar. For more information, visit www.nyp.org and www.med.cornell.edu.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
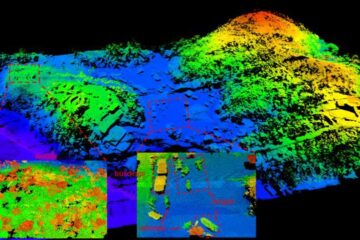
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















