Fat a culprit in fibrotic lung damage

Pulmonary fibrosis has no cure. It's caused by scarring that seems to feed on itself, with the tougher, less elastic tissue replacing the ever moving and stretching lung, making it increasingly difficult for patients to breathe.
Researchers debate whether the lung tissue is directly damaged, or whether immune cells initiate the scarring process – an important distinction when trying to find new ways to battle the disease. Now research shows that both processes may be important, and suggest a new direction for developing novel therapies. The work will publish online November 20th in the American Journal of Respiratory Cell and Molecular Biology.
“By changing our focus, not just to lung cells or immune cells, but to how these cells might be communicating, we may find new opportunities for treating pulmonary fibrosis,” says Ross Summer, M.D., Associate Professor of in the department of Pulmonary and Critical Care Medicine at Thomas Jefferson University, who studies the disease and regularly treats patient with this illness.
“In the advanced stages of the disease, there's not a lot we can do for patients,” says Dr. Summer. Some existing therapies alleviate symptoms, but none reverse or stop disease progression. Many patients live only three to five years after diagnosis, according to the American Lung Association and the only effective treatment is lung transplant.
The team led by Dr. Summer and first author Freddy Romero, Ph.D., looked at a mouse model of lung fibrosis initiated by a chemical known to cause the disease. Researchers noticed that lipids (AKA fat), accumulated within the airspaces of the lung where oxygen is absorbed. Although lipids are normally secreted there to help keep the cells lining the lungs lubricated and properly inflated, these were excessive levels of fat.
The researchers showed that in response to stress, the cells producing the lubricant dump their lipid stores into the lungs and fail to mop up the excess. The excess lipids react with oxygen to create a form of fat that acts as an inflammatory signal; in some ways this response is similar to the events that initiate atherosclerosis, or plaque formation in blood vessels.
In the lungs, Dr. Summer's laboratory showed that immune cells called macrophages, which normally survey the lung for debris, infection, or dying cells begin gobbling up the excess fat in the lungs. Loaded with this oxidized fat, the macrophages turned on a program that acts to help heal the wounded tissue, but as a consequence to this adaptive response leads to the development of fibrotic lung disease.
“Both the initial damage to the cells lining the airway of the lung and the inflammation are important,” says Dr. Romero, “but the thing that drives the damage is the unregulated excess lipids in the distal airspaces.” When the researchers put oxidized lipids into the lungs of mice that had not been exposed to any lung-damaging chemicals, the mice also developed fibrosis, showing that the oxidized fat alone was enough to cause the disease.
“These results show, for the first time, that a break-down of normal lipid handling may be behind this lung disease,” says Dr. Summer “If we prove that the same process holds true in humans, it suggests that we could prevent or mitigate the disease by simply clearing out the excess oxidized lipids from lungs.”
To this end, the researchers tested whether treating mice with an agent called GM-CSF that reduces lipid secretion and facilitates lipid removal in the lungs, could minimize lung fibrosis. Indeed, this agent reduced the scarring in the lungs by over 50 percent based on the levels of lung collagen, a marker of newly forming scar tissue. In addition, the researchers examined human cells in the lab and saw that oxidized fat also promoted a fibrotic response.
Future work will focus on exploring whether the same results hold true in humans.
Research was supported by funding from the National Institutes of Health (NIH) R01HL105490 and by the Intramural Research Program of the National Institutes of Health, National Institute of Environmental Health Sciences grant Z01 ES102005.
The authors report no conflicts of interest.
For more information, contact Edyta Zielinska.
About Jefferson — Health is all we do.
Thomas Jefferson University, Thomas Jefferson University Hospitals and Jefferson University Physicians are partners in providing the highest-quality, compassionate clinical care for patients, educating the health professionals of tomorrow, and discovering new treatments and therapies that will define the future of healthcare. Thomas Jefferson University enrolls more than 3,600 future physicians, scientists and healthcare professionals in the Sidney Kimmel Medical College (SKMC); Jefferson Schools of Health Professions, Nursing, Pharmacy, Population Health; and the Graduate School of Biomedical Sciences, and is home of the National Cancer Institute (NCI)-designated Sidney Kimmel Cancer Center. Jefferson University Physicians is a multi-specialty physician practice consisting of over 650 SKMC full-time faculty. Thomas Jefferson University Hospitals is the largest freestanding academic medical center in Philadelphia. Services are provided at five locations — Thomas Jefferson University Hospital and Jefferson Hospital for Neuroscience in Center City Philadelphia; Methodist Hospital in South Philadelphia; Jefferson at the Navy Yard; and Jefferson at Voorhees in South Jersey.
Article Reference
F. Romero et al., “A pneumocyte-macrophage paracrine lipid axis drives the lung toward fibrosis,” Am J Respir Cell Mol Biol, DOI: 10.1165/rcmb.2014-0343OC, 2014.
Media Contact
More Information:
http://www.jefferson.edu/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
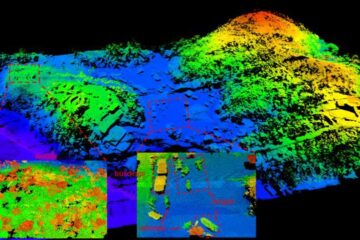
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















