First birth using PGD to save baby from rhesus blood disease

Australian researchers (Thursday 20 January) announced that they have used pre-implantation genetic diagnosis (PGD) to avoid a couple having a baby suffering from rhesus factor[1] disease – the potentially fatal condition caused by incompatibility between a baby’s blood and that of its mother.
Their pioneering work resulted in the birth of a healthy baby girl in November 2003 to a couple who had previously had one child severely affected by Rh disease.
Writing in Europe’s leading reproductive medicine journal Human Reproduction[2], the research team from the Royal North Shore Hospital and Sydney IVF, state that this is the first reported case of an unaffected pregnancy using PGD to prevent Rh disease.
In Caucasian populations about 17% of pregnant women are RhD negative (RhD-). Of these, around 60% will have a baby who has inherited RhD positive (RhD+) blood from its father. During the first pregnancy, the mother recognises the baby’s blood as ’foreign’ and may develop antibodies against it – usually at delivery. This is called alloimmunization. It doesn’t harm the baby, but it puts future pregnancies involving an RhD+ baby at risk because the antibodies the mother made during her first pregnancy may cross the placenta to her unborn child. The result can be haemolytic disease of the fetus or newborn, which, in extreme cases, causes severe anaemia in the fetus, stillbirth or the death of the baby shortly after birth.
Between one and two in a hundred RhD negative women are at risk of alloimmunization during or immediately after a pregnancy. Over the past 35 years this figure has been cut to about 0.2% by the use of anti-D injections administered in the 28th and 34th week of pregnancy.
However, according to lead researcher Dr Sean Seeho, this still results in a significant number of babies in Australia[3] being affected by RhD alloimmunization because there are around 25,000 RhD+ babies born to about 45,000 RhD- mothers annually. And this excludes women sensitized through other events such as miscarriages, abortions and invasive procedures. In countries where anti-D is not available or guidelines may not be carefully followed, the risk of RhD alloimmunization is higher than in Australia.
“We can treat affected babies before birth by intravascular transfusions and achieve a survival rate of between 70% and 95% depending on circumstances, but that means there is still a significant death rate associated with the condition,” said Dr Seeho, who is a research fellow at the Maternal Fetal Medicine Unit at the Royal North Shore Hospital and a clinical lecturer at the University of Sydney.
“A couple who have had a significantly affected pregnancy are faced with the dilemma of whether or not to attempt further pregnancies, and the tendency for Rh disease to worsen with each subsequent RhD incompatible pregnancy plays a major part in the decision. That was the situation for our couple where their second child had developed serious side effects as a result of alloimmunization.”
Dr Seeho said that PGD has mainly been used since its introduction in 1990 to detect single gene diseases such as cystic fibrosis, or to screen for chromosomal disorders. But, in this case the research team used the technique to select an RhD- embryo from among a number of embryos produced after the mother underwent IVF treatment. The technique involves the biopsy and testing of a single cell from early developing embryos with an unaffected embryo subsequently being transferred to the woman’s womb.
“Although the use of PGD to manage Rh disease has been previously published, to our knowledge this is the first case of an unaffected RhD- baby being born to an RhD- alloimmunized mother using PGD,” said Dr Seeho.
He envisaged that PGD for Rh disease would be most likely to be used in future by couples where there had been a previous severely affected pregnancy involving, for example, a stillbirth, or where the fetus had needed an intravascular transfusion.
“Unfortunately, there are currently very few IVF units in Australia and most probably worldwide that could offer PGD for affected couples due to lack of expertise in PGD or the fact that they don’t offer PGD at all. There are also possible financial barriers because it involves IVF.
“However”, he concluded, “PGD does provide an approach for selected couples who face a high risk of this distressing condition and this latest use also underlines the growing potential of PGD for managing other conditions such as sex-linked disorders, single gene defects and chromosomal aberrations.”
[1] Rh factor: After the A, B, AB and O blood groups, rhesus factor is the most important. The gene making a person rhesus positive (RhD+) is called D and is present in most people. When an RhD+ father produces an RhD+ baby in a rhesus negative (RhD-) mother, the baby’s red blood cells act as antigens causing the mother to produce antibodies against them. The antigens do not normally reach the mother’s blood until labour so are unlikely to harm the first pregnancy, but in subsequent pregnancies the levels of antibodies rise rapidly to a point at which they can destroy the baby’s red blood cells, causing severe problems and even the death of the fetus or newborn. Anti-D immunization of the mother can normally prevent the problem. About 16% of Europeans are RhD-. In the USA the figure is 15%, although only 5 to 10% of African Americans are RhD-. Among Africans and Asians, less than 1% are RhD-.
[2] The role of preimplantation genetic diagnosis in the management of severe rhesus alloimmunization: first unaffected pregnancy. Human Reproduction. Doi:10.1092/humrep/deh624.
[3] In England and Wales an estimated 62,000 babies RhD+ babies are born to RhD- mothers every year. Of these, around 500 develop haemolytic disease of the newborn (HND) and 25-30 die of it. About 15 will have permanent developmental problems and 30 will have minor developmental problems. Source: Omar Ali, Hospital Pharmacist, March 2003. In the USA around 4,000 babies are born each year with HND.
Media Contact
More Information:
http://www.eshre.comAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
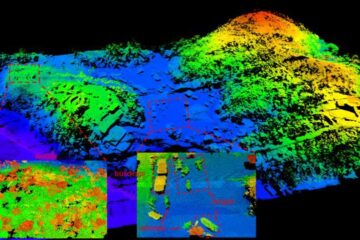
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















