Longterm immune memory cells cells do not develop during chronic viral infections

Finding by Emory University scientists has implications for vaccines, antiviral therapies and cancer treatment
Immune T cells that respond to chronic viral infections do not acquire the same “memory” capabilities of T cells that respond to acute viral infections, according to research by scientists at Emory University. The finding may explain why people lose their immunity to some viruses after chronic infections are controlled. It could guide scientists in developing better therapeutic combinations of antiviral therapies and therapeutic vaccines. The research is published online in the Proceedings of the National Academy of Sciences.
Lead author of the study is E. John Wherry, PhD, postdoctoral fellow in the Department of Microbiology and Immunology at Emory University School of Medicine and the Emory Vaccine Center. Senior author is Rafi Ahmed, PhD, director of the Emory Vaccine Center, Georgia Research Alliance Eminent Scholar, and professor of microbiology and immunology.
The immune system responds to viral infections in two ways: with antibodies that help prevent viruses from entering cells and with T cells activated in response to viral antigens. T cells kill the virus-infected cells and produce proteins called cytokines that prevent the growth of viruses and make cells resistant to viral infection. During the acute phase of a viral infection, activated CD8 T cells respond aggressively for a few weeks, then about five percent of them become “memory cells” that maintain a stable memory T cell population by slow, steady turnover. These memory cells are poised to mount an even stronger and more rapid response to future attacks by the same virus. Individuals who acquire immunity to diseases such as measles, yellow fever, smallpox, or polio, either through exposure or vaccination, often are capable of retaining that immunity for many years or for an entire lifetime.
Dr. Ahmed and his colleagues discovered in previous research that following acute viral infections, immune memory CD8 T cells continue to maintain their ability to attack viruses even when they are not continuously stimulated by viral antigen (Science, Nov. 12, 1999). Other studies have suggested, however, that during some chronic infections continuing exposure to viral antigen may be necessary to maintain protective immunity.
The Emory researchers used a mouse model of infection with lymphocytic choriomeningitis virus (LCMV) to study the differences in CD8 memory T cell immune response following acute and chronic infections. In mice with the acute infection, the virus was cleared by a CD8 T cell immune response within one week. In mice with the chronic infection, high virus levels were present in multiple tissues for the first two to three months, then the virus was controlled in most tissues by a T cell response but was not completely eliminated.
To directly compare the memory capabilities of cells from both types of infection, the scientists transferred both acute memory and chronic memory CD8 T cells into uninfected mice, without transferring any of the viral antigen. The acute memory cells were maintained through homeostasis and divided several times, but the chronic memory cells failed to divide and declined in number over time. When the chronic memory CD8 T cells were transferred back into chronically infected mice where they re-encountered antigen, the cells began to recover.
The scientists also compared other important qualities of memory T cells, including the responsiveness to cytokine signaling by interleukin 7 (IL-7) and interleukin 15 (IL-15). Response to these cytokines is a critical part of the immune pathway that allows memory CD8 T cells to undergo homeostatic division and to persist even in the absence of viral antigen. They found that chronic memory CD8 T cells responded poorly to both IL-7 and IL-15, whereas acute memory CD8T cells proliferated in response to both cytokines. Additional research could show whether the defect in chronic memory cell response to IL-7 and IL-15 can be overcome by increasing the expression of these cytokines, or whether other deficiencies in the pathway exist.
“The normal memory CD8 T cell differentiation program that occurs after acute infection results in memory cells that are capable of long-term persistence in the absence of antigen as a result of slow homeostatic proliferation in response to IL-7 and IL-15,” said Dr. Ahmed. “We have shown that during chronic LCMV infection this memory pathway does not proceed efficiently and that virus-specific CD8 T cells do not acquire the cardinal property of antigen-independent persistence.”
The Emory scientists also concluded that rest from antigen exposure is an important criterion for developing long-term immune memory. Acute memory T cells are exposed to antigen for a finite time period after an acute infection, then after the virus with antigen is eliminated, these cells differentiate into memory T cells. A recent study of HIV infection showed that if antiretroviral therapy is initiated during the early phase of infection, HIV-specific CD8 T cells are maintained more efficiently.
“Our research shows that prolonged exposure to antigen without any rest results in cells that are “addicted” to antigen and cannot persist without it,” Dr. Ahmed explains. “This raises concerns about vaccine strategies that use persisting antigen, because antigen-independent memory T cells may not develop.”
The study may help explain the loss of T cell immunity seen in some chronic infections that are eventually controlled and eliminated, and the ability of some persistent tumors to provide protection from a secondary tumor challenge if the original tumor is not removed. “Giving T cells a rest by terminating exposure to viral antigen simulation following the acute phase of infection seems to be necessary if T cells are to differentiate into long-term antigen-independent memory T cells,” Dr. Ahmed says. “Therapeutic vaccine approaches that provide antigen re-stimulation during persistent infections may not allow the ability for memory T-cell proliferation. However, antiviral therapy or cancer chemotherapy may provide rest from antigen stimulation and allow partial recovery of some memory T cell functions. By combining drug treatment with therapeutic vaccination or cytokine therapies we may be able to prevent loss of T cell memory and establish long-term protective immunity.”
Media Contact
More Information:
http://www.emory.eduAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
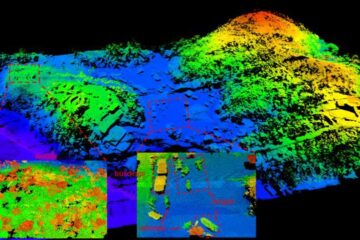
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















