NARSAD researchers identify specific genes and family traits linked to mental illnesses

New Findings Provide Important Clues Toward the Development of Customized Treatments
New findings from research supported by NARSAD, the world’s leading charity dedicated to mental health research, and conducted by Harvard-affiliated scientists are providing important clues into how genes work to impair various aspects of attention, memory and perception — the behaviors associated with many psychiatric illnesses, such as schizophrenia, bipolar disorder and depression.
Presented at NARSAD’s 3rd annual Boston Mental Health Research Symposium on May 30 at the Harvard Medical School, the studies shed new light on how specific genes contribute to the susceptibility to and pathology of schizophrenia, bipolar disorder and depression, some of the most severe, chronic and disabling mental illnesses that collectively affect an estimated 40 million Americans. Coming at a time when some treatments for mental illnesses are a matter of trial and error, these findings have relevance in the development of novel therapies targeted to specific patients and to specific genes.
Donald C. Goff, M.D., director of the Schizophrenia Clinical and Research Program at Massachusetts General Hospital and a leading researcher on the role of genetics in the development of new treatments for schizophrenia, moderated the discussion.
Folate as a Cause and Treatment for Schizophrenia: Who Will Benefit?
Do genes explain why some people with schizophrenia are helped when they take supplements of the common B vitamin, folate? The answer is yes and now, new NARSAD funded research is examining the reasons why.
According to Dr. Goff, whose pioneering research identified a link between low blood levels of folate and negative schizophrenia symptoms, folate is involved in many different chemical pathways in the brain, including keeping levels of the amino acid homocysteine low. When homocysteine levels are too high, this interferes with the functioning of receptors located all over the brain — called NMDA ( N-methyl-D-aspartate) receptors — that are critical to learning, memory, brain development, and general neural processing.
However, what causes low folate in people with schizophrenia is still open to question. One reason, confirmed by epidemiological studies, is poor dietary intake. Based on examining two major famines in the 20th century — the Dutch Hunger Winter of 1944-45 brought about by the Nazi occupation in World War II and the Chinese famine in 1959-61 — scientists found that the incidence of schizophrenia among children born to women who were pregnant during these famines increased two-fold.
But in most cases, starvation is not the problem. That is why Dr. Goff’s team looked for other causes, including two genes: GCPII (glutamate carboxypeptidase II), which controls the absorption of folate and may be deficient in people with schizophrenia, and MTHFR (methylenetetrahydrofolate reductase), which activates folate for use in the brain. Using this information, Dr. Goff and his colleagues are recruiting patients for a large trial to determine whether folate supplementation will help individuals affected by these genes, many of whom have treatment-resistant psychotic symptoms. Funded by the National Institute of Mental Health, this double-blind study will follow 150 patients with schizophrenia at three sites over a 16-week period.
“Schizophrenia is a prevalent and costly disorder and can be very difficult to treat. This is especially true for the estimated 30 percent of patients with treatment-resistant psychotic symptoms, who may also experience social withdrawal, apathy, and depression,” Dr. Goff said. “Having these new data will validate whether folate, which is known to be very safe, is an effective way to improve outcomes for people with schizophrenia who now suffer from treatment-resistant psychotic symptoms.”
Building on this landmark research, scientist and colleague, Joshua Roffman, M.D., is using NARSAD funds to go the next step — identifying people with schizophrenia who are most likely to benefit from folate supplementation. Here, Dr. Roffman and his colleagues started with the MTHFR gene and found that one variant increases the severity of schizophrenia symptoms. Moreover, in patients with this variant, low folate intake was associated with symptoms that were especially severe.
Now, Dr. Roffman’s team is looking at the combination of MTHFR and another gene — COMT (catechol-O-methyltransferase) — that affects dopamine levels in the brain. Although the two genes have separately been associated with schizophrenia, Dr. Roffman’s just completed study finds that when these genes interact, a specific subset of patients is at greater risk for cognitive impairment. In individuals who carry the risk variants of both MTHFR and COMT, lower-than-normal levels of dopamine in the part of the brain called the prefrontal cortex may cause problems with information processing and working memory. Using functional neuroimaging, Dr. Roffman and his colleagues also found that the same combination of MTHFR and COMT variants were associated with abnormally low activity in the prefrontal cortex.
“We now have the techniques to determine how genes combine to produce schizophrenia symptoms,” Dr. Roffman explained. “As we gain a better understanding of individual biogenetic pathways, we can identify high-risk groups and those most likely to benefit from specific treatments.”
Genes and Depression
If a better understanding of genes may lead to customized therapies for schizophrenia, can the same be true for new depression treatments? Answering this question is especially important now that a 2006 government study found that a significant number of people with clinical depression – more than half – are not helped by their initial course of antidepressant treatment, whether medication or talk therapy. In addition, antidepressant medications often come with troubling side effects, such as sleep changes, sexual problems, headaches and gastrointestinal problems, and an analysis by the Food and Drug Administration has shown that antidepressants may cause suicidal thinking and behavior in children, adolescents and adults ages 18 to 24.
According to Roy Perlis, M.D., M.Sc., the director of pharmacogenomics research at Massachusetts General Hospital’s Department of Psychiatry, specific genes may influence how individual patients respond to antidepressant therapies, which is why his research team is using NARSAD funds to try to find these genes.
After studies in mice identified variations of four genes that may affect how individuals respond to antidepressant treatment, Dr. Perlis and his colleagues examined these four genes in DNA samples provided by 1,554 people participating in a large government study called the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial. What the team found was a link between a variation in the gene TREK1 and poorer response to antidepressant treatment. This is especially significant because people with depression often require more than one treatment before they find one that “works” for them. If individuals with more “treatment-resistant” depression can be identified early in their illness, they may be treated more effectively. Further, Dr. Perlis believes that studying how variations in genes affect response to medications will also lead to a completely new class of more targeted antidepressant therapies.
“Our hope is that one day, we will be able to match patients to those treatments that are most likely to be effective,” Dr. Perlis noted. “When we understand how people respond to different treatments and why, we will be able to design more targeted therapies for depression.”
Family Traits Provide Clues to Genes for Schizophrenia, Bipolar Disorder
It is also important to identify the endophenotypes — traits associated with a clinical disorder — that can serve as a roadmap for detecting disease-related genes. That is why Deborah L. Levy, Ph.D., associate professor of psychology in the Department of Psychiatry at Harvard Medical School and director of the Psychology Research Laboratory at McLean Hospital, is studying families to detect relatives who are carriers of the genes for schizophrenia and bipolar disorder, even though these individuals don’t have the diseases themselves.
“One of the key issues in any genetic study is to distinguish individuals who are gene carriers from individuals who are not gene carriers,” explained Dr. Levy. In single gene disorders, such as cystic fibrosis and Huntington's disease, 25 percent and 50 percent of family members, respectively, have the same illness. In contrast, only 6.5 percent of family members of people with schizophrenia actually have the illness, which means most relatives don’t have symptoms of the illness but may still be gene carriers.
To find the relatives who are likely carriers of genes for schizophrenia and bipolar disorder, Dr. Levy and her colleagues have zeroed in on four discernable schizophrenia-related traits that occur in well family members at a much higher rate than schizophrenia itself: difficulty following a slow moving target with one’s eyes, syntax errors or idiosyncratic use of language, subtle anomalies involving the midline of the face , and difficulty filtering out noises and other irrelevant stimuli (a condition known as sensory gating).
These traits, according to Dr. Levy, are much more common in families with schizophrenia. For example, idiosyncratic use of language (a trait similar to the thought disorder observed in schizophrenia) occurs in 37 percent of clinically unaffected first-degree relatives of individuals with schizophrenia, a rate that is almost six times higher than schizophrenia in the same families. When the rates for thought disorder and schizophrenia and related clinical conditions are combined, the proportion of potential gene-carrying relatives is close to 50 percent, consistent with a dominant gene, and much higher than the 6.5 percent rate of schizophrenia in the same families.
“With diseases like schizophrenia and bipolar disorder, identifying the genes is just the starting point,” noted Dr. Levy. “The ultimate goal is to discover the biological processes these genes initiate in the brain, ultimately leading to better treatments in the future.”
About NARSAD
NARSAD’s Boston Mental Health Symposium is one of several such programs the organization presents annually around the country to bring the latest developments in research to the attention of the public.
NARSAD’s primary mission is to raise funds to advance research on the causes, treatment and prevention of psychiatric disorders. Since it began giving grants in 1987, as the National Alliance for Research on Schizophrenia and Depression, NARSAD has awarded more than $234 million in competitive grants to nearly 2,700 scientists at leading universities, medical centers and research institutions around the world who are conducting research on schizophrenia, depression, bipolar disorder, anxiety disorders, childhood mental disorders and other serious mental illnesses.
For additional information on the work of NARSAD, the research it supports, and various psychiatric disorders, visit the organization’s Web site at www.narsad.org or call 800-829-8289.
Media Contact
More Information:
http://www.narsad.orgAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
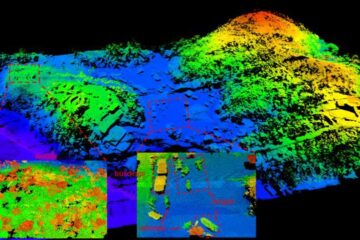
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















