Cell surface transporters exploited for cancer drug delivery

Although this finding emerges from the study of a single toxic molecule and the protein that it transports, Whitehead Member David Sabatini says this phenomenon could be leveraged more broadly.
“Our work suggests a different strategy for cancer therapy that takes advantage of the capacity of a cancer cell to take up something toxic that a normal cell does not,” says Sabatini, who is also a professor of biology at MIT and a Howard Hughes Medical Institute (HHMI) investigator. “As a result, that toxic molecule would kill the cancer cell. By identifying transporters on the surface of cancer cells, you might be able to find a molecule that a specific transporter would carry into the cell, and that molecule would be toxic to that cell. You really could have something that's much more selective to cancer cells.”
The Sabatini lab's research is published online today in the journal Nature Genetics.
Kivanc Birsoy, a postdoctoral researcher in Sabatini's lab and first author of the Nature Genetics paper, used a special line of haploid cells developed by former Whitehead Fellow Thijn Brummelkamp to screen for genes that assist cellular entry of 3-bromopyruvate's (3-BrPA), a potential cancer drug in clinical development. 3-BrPA is thought to work by inhibiting glycolysis, a cellular process that releases energy by splitting glucose molecules. Because many cancer cells are heavily dependent on the upregulation of glycolysis, drugs that interrupt this pathway may be effective in targeting these glycolytic cancer cells.
From the screen and massively parallel sequencing, Birsoy identified the gene that codes for the protein monocarboxylate transporter 1 (MCT1), which is necessary and sufficient for 3-BrPA's transport into cells, where the toxic molecule ultimately kills them. In fact, the level of MCT1 on the surface of glycolytic tumor cells is a predictor of those cells' sensitivity to 3-BrPA—the higher the cells' expression of MCT1, the more sensitive they are to 3-BrPA. This holds true in in vitro and in vivo models across multiple lines of human cancer cells.
The correlation between MCT1 concentration and 3-BrPA sensitivity could be used to help determine how certain malignant tumors are treated.
“This study makes MCT1 a biomarker for 3-BrPA,” says Birsoy. “So in the future, if 3-BrPA is approved as a drug, presumably you could predict if a patient's cancer tumor is going to be sensitive by looking at the levels of this molecule. No tumor without MCT1 would respond to treatment with 3-BrPA.”
This work was supported by the National Institutes of Health (CA103866), the David H. Koch Institute for Integrative Cancer Research, the Jane Coffin Childs Memorial Fund, and the National Science Foundation (NSF).
Written by Nicole Giese Rura
David Sabatini's primary affiliation is with Whitehead Institute for Biomedical Research, where his laboratory is located and all his research is conducted. He is also a Howard Hughes Medical Institute investigator and a professor of biology at Massachusetts Institute of Technology.
Full Citation:
“MCT1-mediated transport of a toxic molecule is an effective strategy for targeting glycolytic tumors”
Nature Genetics, December 2, 2012, online.
Kivanc Birsoy (1,2), Tim Wang (1), Richard Possemato (1,2), Omer H Yilmaz (1,2), Catherine E Koch (1,2), Walter W Chen (1,2), Amanda W Hutchins (1,2), Yetis Gultekin (1,2), Tim R Peterson (1,2), Jan E Carette (1,6), Thijn R Brummelkamp (1,6), Clary B Clish (3) and David M Sabatini (1).
1. Whitehead Institute for Biomedical Research, Cambridge, Massachusetts, USA.
2. Department of Biology, Massachusetts Institute of Technology (MIT), Cambridge, Massachusetts, USA.
3. Broad Institute, Cambridge, Massachusetts, USA.
4. David H Koch Institute for Integrative Cancer Research at MIT, Cambridge, Massachusetts, USA.
5. Howard Hughes Medical Institute, MIT, Cambridge, Massachusetts, USA.
6. Present addresses: Department of Microbiology and Immunology, Stanford University School of Medicine, Stanford, California, USA (J.E.C.) and Department of Biochemistry, Netherlands Cancer Institute, Amsterdam, The Netherlands (T.R.B.)
Media Contact
More Information:
http://www.wi.mit.eduAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
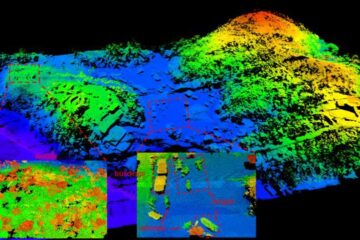
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















