Cedars-Sinai, global consortium develop stem cell tool to test Huntington’s treatments

Cedars-Sinai scientists, in collaboration with expert colleagues around the globe, used stem cells to re-create Huntington’s Disease in a petri dish, allowing researchers for the first time to test potential treatments for the fatal inherited neurological disorder directly on human cells.
As outlined in a paper published online by Cell Stem Cell and slated for print in the journal’s Aug. 3 issue, scientists at Cedars-Sinai’s Regenerative Medicine Institute and the University of Wisconsin took skin cells from patients with Huntington’s disease and reprogrammed them into powerful stem cells; these were then made into the nervous system cells affected by the disease. Seven laboratories around the world collaborated to demonstrate the cells had hallmarks of Huntington’s.
“Now that we’ve moved from skin cells to brain cells, the next step forward will be to test treatments we can move from the petri dish to the clinic,” said Clive Svendsen, PhD, director of the Cedars-Sinai Regenerative Medicine Institute and a senior author of the study. “In addition to increasing our understanding of this disorder and offering a new pathway to identifying treatments, this study is remarkable because of the extensive interactions between a large group of scientists focused on developing this model. It’s a new way of doing trailblazing science.”
This breakthrough is the latest example of an innovative use for stem cells, reprogramming them to create laboratory versions of diseases. This method has been used to mimic Parkinson’s disease, Alzheimer’s disease, ALS and spinal muscular atrophy. As these diseases all occur in living neurons – that patients can’t part with – the disease-in-a-dish models offer scientists an opportunity they never had before: to study in human cells how a disease attacks the neurons and plot strategies for fighting it.
The Huntington’s Disease iPSC Consortium united some of the world’s top scientists working on this disease. Cedars-Sinai researchers took skin cells from a several Huntington’s patients, including a six-year-old with a severe juvenile form of the disease. They genetically reprogrammed these tissues into induced pluripotent stem cells, which can be made into any type of cell in the body. The cells lines were banked by scientists at Cedars-Sinai and scrutinized by all consortium members for differences that may have led to the disease. These cell lines are now an important resource for Huntington’s researchers and have been made available via a National Institutes of Health-funded repository at Coriell Institute for Medical Research in New Jersey.
Huntington’s, known to the public, for example, as the cause of folksinger Woody Guthrie’s death, typically strikes patients in midlife. It causes jerky, twitching motions, loss of muscle control, psychiatric disorders and dementia; the disease ultimately is fatal. In rare, severe cases, the disorder appears in childhood.
Researchers believe that Huntington’s results from a mutation in the huntintin gene, leading to production of an abnormal protein and ultimately cell death in specific areas of the brain that control movement and cognition. There is no cure for Huntington’s, nor therapies to slow its progression.
The consortium showed Huntington’s cell deficits or how they differ from normal cells, including that they were less likely to survive cultivation in the petri dish. Scientists tried depriving them of a growth factor present around normal cells, or “stressing” them, and found that Huntington’s neurons died even faster. The trick with disease-in-a-dish models is verifying that the cells are, in fact, behaving in the same manner they would in a patient, said Virginia Mattis, a post-doctoral scientist at the Cedars-Sinai Regenerative Medicine Institute and one of the lead authors of the study.
“It was great that these characteristics were seen not only in our laboratory, but by all of the consortium members using different techniques,” Mattis said. “It was very reassuring and significantly strengthens the value of this study.”
This new model will provide the foundation for a new round of experiments by the consortium funded by a new grant from the NIH and the California Institute for Regenerative Medicine.
The Cedars-Sinai’s Regenerative Medicine Institute has made a major commitment to projects like this Huntington’s study in which stem cell research helps to advance understanding of human disease and open new and innovative methods to identify treatments and cures. The institute has developed an induced pluripotent stem cell core facility and recruited faculty to work in this emerging area of regenerative medicine research.
“At last, we have a human cell model for this tragic disease that will be a powerful new tool in identifying treatments for these patients,” said Shlomo Melmed, MD, dean of the medical faculty at Cedars-Sinai and the Helena A. and Philip E. Hixon Chair in Investigative Medicine. “This development is a compelling example of how important iPS cells are to furthering our understanding and finding cures for diseases that are currently untreatable.”
The consortium includes: Cedars-Sinai Medical Center; Johns Hopkins University School of Medicine in Baltimore; University of California, Irvine; University of Wisconsin School of Medicine; Massachusetts General Hospital; Harvard Medical School; University of California, San Francisco; Cardiff University; Universita degli Studi di Milano; and the CHDI Foundation.
Funding for the research came from an American Recovery and Reinvestment Act grant from the NIH’s National Institute of Neurological Disorders and Stroke (NINDS Recovery Act grant number: RC2-NS069422 ), a grant from the CHDI Foundation, Inc. and CIRM.
Media Contact
More Information:
http://www.cshs.orgAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
High-energy-density aqueous battery based on halogen multi-electron transfer
Traditional non-aqueous lithium-ion batteries have a high energy density, but their safety is compromised due to the flammable organic electrolytes they utilize. Aqueous batteries use water as the solvent for…

First-ever combined heart pump and pig kidney transplant
…gives new hope to patient with terminal illness. Surgeons at NYU Langone Health performed the first-ever combined mechanical heart pump and gene-edited pig kidney transplant surgery in a 54-year-old woman…
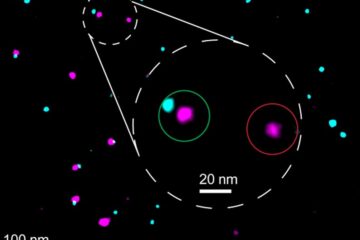
Biophysics: Testing how well biomarkers work
LMU researchers have developed a method to determine how reliably target proteins can be labeled using super-resolution fluorescence microscopy. Modern microscopy techniques make it possible to examine the inner workings…





















