Neurosurgeons at Rush Explore "Smart" Drug to Treat Brain Cancer

The use of a “smart” drug that targets cancer cells in the brain following removal of a tumor may provide treatment that can extend the survival of people with the most common form of primary malignant brain tumor, glioblastoma multiforme (GBM).
A phase III research study being conducted at Rush University Medical Center by neurosurgeon Dr. Richard Byrne involves the use of convection-enhanced delivery, a novel drug delivery approach, to facilitate infusion of the study drug, IL13-PE38QQR, into the brain. IL13-PE38QQR is designed to attach to specific receptors on tumor cells that are not present on normal brain cells.
The problem with current treatments for brain tumors is that while neurosurgeons can remove as much as 95 percent or more of a tumor, some cancer cells will remain undetectable and scattered throughout the brain tissue adjacent to the tumor site. Current methods to kill the remaining cancer cells with radiation or chemotherapy have resulted in a median survival rate after initial diagnosis of about nine to twelve months, and normal brain cells can be injured in the process.
Patients in the study first will undergo neurosurgery to remove as much of the GBM tumor as possible. Within a week, magnetic resonance imaging (MRI) will be used to scan the brain tissue around the cavity where the tumor has been removed to identify suspicious areas where cancer cells may remain.
With the target areas identified, Byrne and his team will then perform a second surgical procedure using an image guidance technique to pass catheters through the skull into the brain to reach two to four areas of tissue suspected of harboring residual, infiltrating tumor cells. Following catheter placement, the drug is continually infused or delivered through the catheters into the brain. A pump is used to slowly push the drug solution through the catheters. This method of treatment is referred to as convection-enhanced delivery, or CED. The patient is able to walk around during this time.
IL13-PE38QQR is a hybrid protein that contains the cytokine IL13, which allows the drug to specifically attach or bind to tumor cells that have the IL13 receptor. “Like a key to a lock,” the cytokine binds to the receptor and allows the study drug to enter and potentially kill the tumor cells. Normal brain cells remain unaffected because they do not appear to have the IL13 receptor and therefore the study drug does not bind to them.
The positive-pressure, convection-enhanced delivery method is used to diffuse the drug throughout the targeted brain tissue. Convection enhanced delivery to brain tissue allows the drug to bypass the blood-brain barrier, which protects the brain by preventing “foreign substances” such as drugs in the blood from reaching brain tissue, which can occur when drugs are administered systemically. “There are countless success stories of treating tumors that work in cell lines that fail when we try them in the brain, in part because of the blood brain barrier,” said Byrne, who is a member of the Chicago Institute of Neurosurgery and Neuroresearch medical group (CINN). He is the principal investigator for the study at Rush.
“Previous studies with this drug have shown that it was safe and that there were some very dramatic responses in terms of eliminating residual tumor in the brain and prolonging patient life. We believe this drug can positively improve life span for some GBM brain tumor patients by destroying the cancerous cells we cannot remove through neurosurgery,” said Byrne.
One-third of the patients enrolled in the trial will be randomly assigned to receive one treatment currently available. These patients will undergo surgery to remove the tumor and to have FDA approved chemotherapeutic “wafers” placed in the tumor cavity. The wafers slowly dissolve over 2 to 3 weeks, releasing chemotherapeutic drugs to the area. Two-thirds of the study patients will be randomly assigned to receive the IL13-PE38QQR study drug.
GBM is the most common and aggressive form of primary brain tumors, and most cases occur in people between the ages 40 and 60. GBM is a highly malignant tumor and infiltrates the normal brain tissue surrounding the tumor. GBMs may also invade the membranes covering the brain, or spread via the spinal fluid bathing the brain and spinal cord. Most malignant gliomas are known to re-grow in a location close to the resection cavity left by the removal of the tumor.
People with these brain tumors typically suffer from some degree of symptoms that can include headaches, nausea and vomiting, personality changes, seizures, vision loss and slowing of cognitive function.
Individuals interested in participating in this study must have a diagnosis of recurrent glioblastoma multiforme and the tumor must have reoccurred after surgical resection, radiation and chemotherapy were used to treat the initial tumor.
The “PRECISE” (Phase III Randomized Evaluation of Convection IL13) trial is designed to enroll up to 300 patients. A number of the world’s leading brain tumor treatment centers, including Rush University Medical Center, have agreed to participate in the PRECISE trial to further the study of treatments for GBM. NeoPharm, Inc., based in Lake Forest, Ill., funds the study and supplies the IL13-PE338, which was developed in the Laboratory of Molecular Tumor Biology of the U.S. Food and Drug Administration.
Media Contact
More Information:
http://www.rush.eduAll latest news from the category: Agricultural and Forestry Science
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
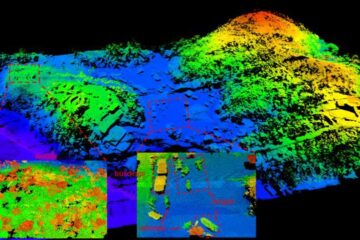
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















