Killer T Cells Support Tissue Regeneration
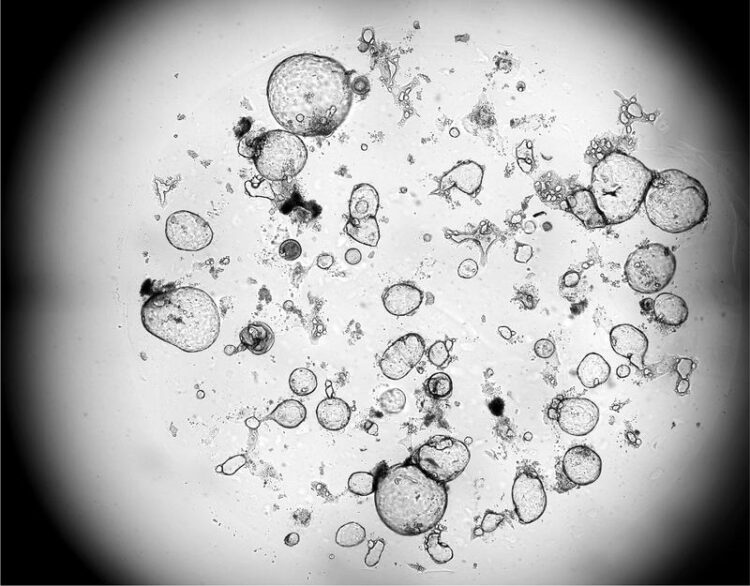
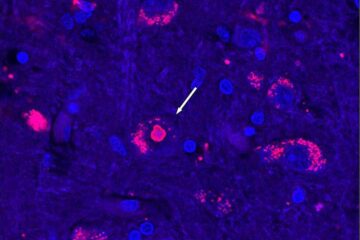
Released factors from activated killer T cells promote the growth of human mini-organs (organoids).
(c) LIT
Researchers at the Leibniz Institute for Immunotherapy (LIT) have demonstrated that killer T cells of the immune system not only eliminate pathologically altered cells, but also promote the subsequent tissue wound healing process.
One of the main functions of the immune system is to defend the body against infections or cancer. This task is efficiently carried out by immune cells known as killer T cells. These cells possess the ability to destroy body cells that are, for example, infected by viruses or transformed into tumor cells. However, what happens after the destruction of infected body cells? How is tissue damage, resulting from the destruction of target cells, repaired, and organ function restored? These questions were examined in detail by the Immunology Division of the LIT.
“In wound healing experiments with human virus-specific killer T cells we observed that after the destruction of infected cells, neighboring cells began to divide and fill the gap,” describes Michael Delacher, one of the main authors of the study. In the experiments, a wound was created in a seeded cell layer. Culture supernatants from activated killer T cells caused this wound to close quickly. “This indicates that soluble factors produced by killer T cells during the destruction of infected cells support the healing of the remaining tissue cells,” explains main author Lisa Schmidleithner.
Which factors mediate this surprising healing property? The authors found that growth factors such as amphiregulin are involved in the wound healing effect. Human killer T cells can produce these growth factors and stimulate other cells in the tissue to produce them as well. In addition to these growth factors, “classic” immune messengers such as tumor necrosis factor and interferon-gamma can enhance the impact of amphiregulin and support the wound healing effect.
To better understand the impact of the regenerative effects of killer T cells, human mini-organs, called organoids, were co-cultured with killer T cells. “We observed that the number and size of these organoids significantly increased when activated killer T cells or their released growth factors were present,” reports main author Philipp Stüve. This suggests that killer T cell-mediated wound healing processes can influence complex regeneration processes.
In addition to these positive effects on tissue regeneration and wound healing, the same killer T cell-derived growth factors could potentially promote diseases such as cancer. “Indeed, in further experiments, we observed that factors produced by activated killer T cells also enhanced the growth of tumor cells,” reports Malte Simon, one of the main authors of the study.
What do these results mean for further research?
“Our data suggest that killer T cells not only destroy pathologically altered cells but also initiate the subsequent tissue regeneration,” explains Markus Feuerer, the lead author of the study. This mechanism could be useful in the context of viral infections to promote wound closure after the destruction of infected cells and thus restore functionality of the tissue. However, in the context of tumor diseases, this could promote the growth of undestroyed tumor cells. Further research at the LIT must now clarify how to separate the destruction capacity from the wound-healing function of killer T cells. One possible approach is through so-called CAR T cell therapies, where killer T cells are genetically optimized to better destroy tumors. In the cell engineering process, it might be possible to delete the wound-healing capabilities of killer T cells.
The Leibniz Institute for Immunotherapy (LIT) is an institute within the Leibniz Association located in Regensburg, Germany. Our mission is to develop innovative therapies for the treatment of cancer, autoimmunity, and chronic inflammation. By reprogramming immune cells through synthetic and pharmacological strategies, we build cells that save lives.
Wissenschaftliche Ansprechpartner:
Prof. Dr. Markus Feuerer
Head, Division of Immunology
LIT – Leibniz Institute for Immunotherapy
c/o University Hospital Regensburg
Franz-Josef-Strauss-Allee 11
93053 Regensburg, Germany
phone: +49 941 944 38121
email: markus.feuerer@ukr.de
Professor of Immunology
Head, Chair for Immunology
University of Regensburg
Originalpublikation:
Journal of Experimental Medicine
https://doi.org/10.1084/jem.20230488
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Recovering phosphorus from sewage sludge ash
Chemical and heat treatment of sewage sludge can recover phosphorus in a process that could help address the problem of diminishing supplies of phosphorus ores. Valuable supplies of phosphorus could…

Efficient, sustainable and cost-effective hybrid energy storage system for modern power grids
EU project HyFlow: Over three years of research, the consortium of the EU project HyFlow has successfully developed a highly efficient, sustainable, and cost-effective hybrid energy storage system (HESS) that…
After 25 years, researchers uncover genetic cause of rare neurological disease
Some families call it a trial of faith. Others just call it a curse. The progressive neurological disease known as spinocerebellar ataxia 4 (SCA4) is a rare condition, but its…





















