Personalized approach to smoking cessation may be reality in 3-5 years

“Within three to five years, it's conceivable we'll have a practical test that could take the guesswork out of choosing a smoking-cessation therapy,” says Jed Rose, Ph.D., director of Duke's Center for Nicotine and Smoking Cessation Research. “It could be used by clinicians to guide the selection of treatment and appropriate dose for each smoker, and hopefully increase cessation success rates.”
Statistics show 70 percent of the nation's 46 million smokers say they want to quit, yet successfully kicking the habit has not proven easy. In previously published reports, less than five percent of smokers who tried to quit on their own without any aids were not smoking one year later. Long-term quit rates for smokers who relied on pharmacological intervention hover under 25 percent.
The research, which is published online in the July-August issue of Molecular Medicine, follows previous work done by Rose and George Uhl, MD PhD, chief of the molecular neurobiology research at NIDA. After conducting a genome-wide scan of 520,000 genetic markers taken from blood samples of smokers in several quit-smoking trials, they identified genetic patterns that appear to influence how well individuals respond to specific smoking cessation treatments.
The latest research focuses on combining the information from those individual genetic markers, called SNPs, into one number that represents a “quit success score,” Rose says. The score and the smokers' nicotine dependence, assessed via a simple questionnaire, help predict an individual's likelihood of quitting, as well as whether a high-dose or low-dose nicotine patch would work best.
In the trial, 479 cigarette smokers who smoked at least 10 cigarettes per day and wanted to quit were categorized as either high- or low-dependence based on their level of nicotine dependence. The smokers in each group were then randomly assigned to wear two nicotine skin patches daily delivering a high dose ( (42mg) or a standard dose (21 mg). Patches were worn for two weeks prior to their quit date, and the nicotine doses were reduced gradually over the 10 weeks following their quit date. Participants were given denicotinized cigarettes during the two weeks before the quit date to minimize any potential adverse effects from the high dose nicotine patches. The treatment phase lasted for 12 weeks in all.
DNA was extracted from participants' blood and was used to assess a quit-smoking success genetic score.
At six months follow up, the researchers were able to confirm which smokers fared better or worse on the high-dose compared to the low-dose patch.
“The genotype score was part of what predicted successful abstinence. In the future such a score could help us make our initial treatment decisions,” said Rose. “People who had both high nicotine dependence and a low or unfavorable quit success genetic score seemed to benefit markedly from the high-dose nicotine patch, while people who had less dependence on nicotine did better on the standard patch.”
Further studies are needed to replicate these results, and to expand the research to include therapies like verenicline (Chantix, Pfizer) and bupropion hydrochloride (Zyban, Glaxo SmithKline). But the potential this work holds for the future is significant, Rose says.
“Right now there is no treatment algorithm that tells a clinician or smoker which treatment is likely to work for them,” says Rose. That's what we are trying to do. We want to tailor and give informative guidance to clinicians in terms of what should be tried first to maximize smoking cessation success.”
This study was the result of a collaboration between an investigator supported by the National Institutes of Health (NIH) Intramural Research Program, National Institute on Drug Abuse, and Duke University researchers who received a grant from Philip Morris USA. The company had no role in the planning or execution of the study, data analysis or publication of results.
Disclosure: Drs. Uhl and Rose are listed as inventors for a patent application filed by Duke University based on genomic markers that distinguish successful quitters from unsuccessful quitters in data from other clinical trials.
Media Contact
More Information:
http://www.duke.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
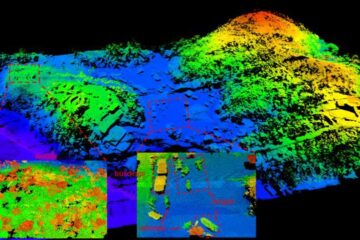
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















