A millimeter-scale, wirelessly powered cardiac device

A team of engineers at Stanford has demonstrated the feasibility of a super-small, implantable cardiac device that gets its power not from batteries, but from radio waves transmitted from outside the body. The implanted device is contained in a cube just eight-tenths of a millimeter in radius. It could fit on the head of pin.
The findings were published in the journal Applied Physics Letters. In their paper, the researchers demonstrated wireless power transfer to a millimeter-sized device implanted five centimeters inside the chest on the surface of the heart—a depth once thought out of reach for wireless power transmission.
The paper's senior author was Ada Poon, a professor of electrical engineering at Stanford. Sanghoek Kim and John Ho, both doctoral candidates in Poon's lab, were first authors.
The engineers say the research is a major step toward a day when all implants are driven wirelessly. Beyond the heart, they believe such devices might include swallowable endoscopes—so-called “pillcams” that travel the digestive tract—permanent pacemakers and precision brain stimulators; virtually any medical applications where device size and power matter.
A revolution in the body
Implantable medical devices in the human body have revolutionized medicine. Hundreds of thousands if not millions of pacemakers, cochlear implants and drug pumps are today helping people live relatively normal lives, but these devices are not without engineering challenges.
First off, they require power, which means batteries, and batteries are bulky. In a device like a pacemaker, the battery alone accounts for as much as half the volume of the device it drives. Second, batteries have finite lives. New surgery is needed when they wane.
“Wireless power solves both challenges,” said Poon.
Last year, Poon made headlines when she demonstrated a wirelessly powered, self-propelled device capable of swimming through the bloodstream. To get there she needed to overturn some long-held assumptions about delivery of wireless power through the human body.
Her device works by a combination inductive and radiative transmission of power. Both are types of electromagnetic transfer in which a transmitter sends radio waves to a coil of wire inside the body. The radio waves produce an electrical current in the coil sufficient to operate a small device.
There is an indirect relationship between the frequency of the transmitted radio waves and the size of the receive antenna. That is, to deliver a desired level of power, lower frequency waves require bigger coils. Higher frequency waves can work with smaller coils.
“For implantable medical devices, therefore, the goal is a high-frequency transmitter and a small receiver, but there is one big hurdle,” explained Kim.
Ignoring consensus
Existing mathematical models have held that high frequency radio waves do not penetrate far enough into human tissue, necessitating the use of low-frequency transmitters and large antennas—too large to be practical for implantable devices.
Ignoring the consensus, Poon proved the models wrong. Human tissue dissipates electric fields quickly, it is true, but radio waves can travel in a different way—as alternating waves of electric and magnetic fields. With the correct equations in hand, she discovered that high-frequency signals travel much deeper than anyone suspected.
“In fact, to achieve greater power efficiency, it is actually advantageous that human tissue is a very poor electrical conductor,” said Kim. “If it were a good conductor, it would absorb energy, create heating and prevent sufficient power from reaching the implant.”
According to their revised models, the researchers found that the maximum power transfer through human tissue occurs at about 1.7 billion cycles per second.
“In this high-frequency range, we can increase power transfer by about ten times over earlier devices,” said Ho, who honed the mathematical models.
The discovery meant that the team could shrink the receive antenna by a factor of ten as well, to a scale that makes wireless implantable devices feasible. At that the optimal frequency, a millimeter-radius coil is capable of harvesting more than 50 microwatts of power, well in excess of the needs of a recently demonstrated eight-microwatt pacemaker.
Additional challenges
With the dimensional challenges solved, the team found themselves bound in by other engineering constraints. First, electronic medical devices must meet stringent health standards established by the IEEE, particularly with regard to tissue heating. Second, the team found that receive and transmit antennas had to be optimally oriented to achieve maximum efficiency. Differences in alignment of just a few degrees could produce troubling drops in power.
“This can't happen with medical devices,” said Poon. “As the human heart and body are in constant motion, solving this issue was critical to the success of our research.”
The team responded by designing an innovative slotted transmit antenna structure. It delivers consistent power efficiency regardless of orientation of the two antennas.
The new design serves additionally to focus the radio waves precisely at the point inside the body where the implanted device rests on the surface of the heart, increasing the electric field where it is needed most, but canceling it elsewhere. This helps reduce overall tissue heating to levels well within the IEEE standards. Poon has applied for a patent for the antenna structure.
This research was made possible by funding from the C2S2 Focus Center, one of six research centers funded under the Focus Center Research Program (FCRP), a Semiconductor Research Corporation entity. Lisa Chen also contributed to this study.
This article was written by Andrew Myers, associate director of communications for the Stanford University School of Engineering.
Media Contact
More Information:
http://www.stanford.eduAll latest news from the category: Medical Engineering
The development of medical equipment, products and technical procedures is characterized by high research and development costs in a variety of fields related to the study of human medicine.
innovations-report provides informative and stimulating reports and articles on topics ranging from imaging processes, cell and tissue techniques, optical techniques, implants, orthopedic aids, clinical and medical office equipment, dialysis systems and x-ray/radiation monitoring devices to endoscopy, ultrasound, surgical techniques, and dental materials.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
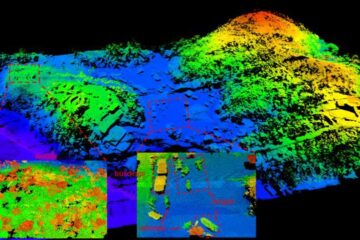
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















