New CPR technique for out-of-hospital cardiac arrest increases survival by 53 percent

The study, which is published in the January 19th, 2011 online version of Lancet, and will be in an upcoming publication of Lancet, determined that active compression-decompression cardio-pulmonary resuscitation (CPR) with augmentation of negative intrathoracic pressure gave patients a better chance of survival. When the pressure inside the thorax decreases, blood flow to the heart and brain increases.
About 800,000 people in the U.S., Canada and Europe have an out-of-hospital cardiac arrest every year. The survival rate averages just 5%, in part because standard CPR is inefficient, providing just 25% of healthy blood flow to the heart and brain.
In the randomized study, 46 emergency medical service (EMS) agencies in urban, suburban and rural areas of the USA, including EMS in Oshkosh, provided either standard CPR or the new technique to adults who had a non-traumatic arrest presumed cardiac in nature.
The new technique uses two devices simultaneously to increase circulation. One is a handheld device that attaches with a small suction cup to the patient's chest. After each compression, the suction cup allows the chest to be lifted up, stimulating blood flow. The second device, called an impedance threshold device, attaches to the patient's airway using a facial mask or breathing tube. When the chest lifts upward, the impedance threshold device prevents air from rushing into the lungs. That creates a vacuum inside the chest and helps refill the heart after each compression. Researchers found in each compression-decompression cycle, the heart and brain receive nearly three times more blood flow when compared with standard CPR.
A total of 813 standard CPR patients and 840 intervention patients were analyzed in the study. Researchers found 6% of the standards CPR patients survived to hospital discharge with favorable neurologic function. That compares with 9% in the intervention group (improvement of survival chance 53% in intervention group). The same proportions of patients in each group survived to one year.
“Based on our findings, active compression-decompression CPR with augmentation of negative intrathoracic pressure should be considered as an alternative to standard CPR to increase long-term survival after cardiac arrest,” said Dr. Aufderheide.
Co-authors on the Lancet paper include Dr. Ralph J. Frascone, MD, Department of Emergency Medicine, Regions Hospital, St. Paul, MN; Dr. Marvin A. Wayne, MD, Whatcom County Emergency Services, Department of Emergency Medicine, Peace Health, St. Joseph Medical Center, Bellingham, WA; Dr. Brian D. Mahoney, MD and Dr. Keith G. Lurie, MD, Department of Emergency Medicine, Hennepin County Medical Center, Minneapolis, MN; Dr. Robert A. Swor, DO, Department of Emergency Medicine, William Beaumont Hospital, Royal Oak, MI; Dr. Robert M Domeier, Department of Emergency Medicine, St. Joseph Mercy Hospital, Ann Arbor, MI; Dr. Michael L. Olinger, MD, Department of Emergency Medicine, Indiana University School of Medicine, Indianapolis, IN; Dr. Richard G. Holcomb, PhD, Quintiles Consulting, Rockville, MD; Dr. David Tupper, PhD and Dr. Demetris Yannopoulos, MD, Departments of Neurology and Medicine—Cardiovascular Division, University of Minnesota Medical Center, Minneapolis, MN.
About The Medical College of Wisconsin
Founded in 1893, the Medical College of Wisconsin is a national, private, academic institution dedicated to leadership and excellence in its fourfold mission: Education, Discovery, Patient Care and Community Engagement. Its core competency is medical knowledge, which underpins every aspect of its mission. As a major national research center, Medical College faculty receives more than $157 million annually in external support for research and training grants. It is home to ten national and international research centers and is recognized as a world leader in research in such areas including heart disease, genetics, obesity, medical imaging and bone marrow transplantation. The Medical College is at the forefront of discovering the genetic influences of complex diseases such as hypertension, renal failure and cancer. The Medical College's 1,200 faculty physicians provide care to more than 390,000 patients annually.
Media Contact
More Information:
http://www.mcw.eduAll latest news from the category: Studies and Analyses
innovations-report maintains a wealth of in-depth studies and analyses from a variety of subject areas including business and finance, medicine and pharmacology, ecology and the environment, energy, communications and media, transportation, work, family and leisure.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
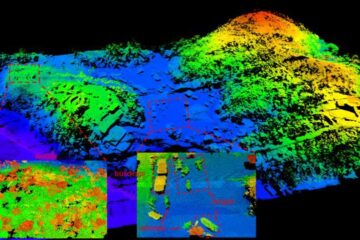
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















