Cancer drug may also work for scleroderma

A drug used to treat cancer may also be effective in diseases that cause scarring of the internal organs or skin, such as pulmonary fibrosis or scleroderma.
The drug, with the generic name bortezomib, stopped the production of fibrotic proteins in human cells and the development of fibrous scarring in a mouse model of fibrotic disease, according to a new Northwestern Medicine study published in the journal Thorax.
“This drug appears to put the brakes on abnormal development of scar tissue in the lungs and skin and may also work in other organs,” said lead author Manu Jain, M.D., associate professor of medicine and of pediatrics at Northwestern University Feinberg School of Medicine and a physician at Northwestern Memorial Hospital and Children's Memorial Hospital. “These diseases have a high fatality rate, and there is no truly effective treatment for them right now.”
Scleroderma is an autoimmune disease that causes progressive thickening and tightening of the skin and can lead to serious internal organ damage and, in some cases, death. Scleroderma affects an estimated 300,000 people in the United States, most frequently young to middle-aged women.
Idiopathic pulmonary fibrosis is a scarring or thickening of the lungs without any known cause that makes it increasingly difficult to breathe. It may affect up to 200,000 people in the U.S. between 50 and 70 years old.
Jain said the drug appears to inhibit a protein called transforming growth factor beta, which is essential for the growth of the scar tissue. Patients with fibrosis have increased levels and activity of the growth factor. Bortezomib is currently used to treat multiple myeloma and lymphoma.
In the study, when researchers gave bortezomib to mice, it prevented the development of a fibrotic-like disease. “The mice that normally get this disease didn't get it,” Jain said.
Researchers also took fibroblast cells from scleroderma and pulmonary fibrosis patients and incubated those cells with the drug. Fibroblast cells are believed to be important in the development of scarring in humans. The drug prevented the expression of proteins that are necessary for scarring.
Coauthors on the study are Gokhan Mutlu, M.D., and Scott Budinger, M.D., both associate professors of medicine at Feinberg and physicians at Northwestern Memorial Hospital.
Media Contact
More Information:
http://www.northwestern.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Webb captures top of iconic horsehead nebula in unprecedented detail
NASA’s James Webb Space Telescope has captured the sharpest infrared images to date of a zoomed-in portion of one of the most distinctive objects in our skies, the Horsehead Nebula….
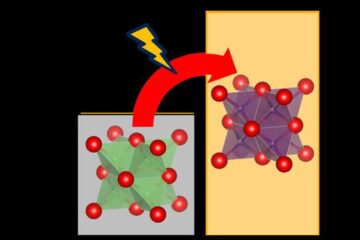
Cost-effective, high-capacity, and cyclable lithium-ion battery cathodes
Charge-recharge cycling of lithium-superrich iron oxide, a cost-effective and high-capacity cathode for new-generation lithium-ion batteries, can be greatly improved by doping with readily available mineral elements. The energy capacity and…
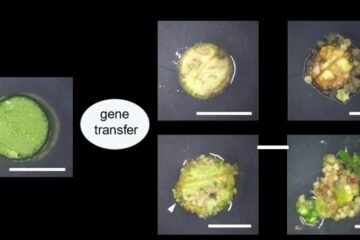
Novel genetic plant regeneration approach
…without the application of phytohormones. Researchers develop a novel plant regeneration approach by modulating the expression of genes that control plant cell differentiation. For ages now, plants have been the…





















