Re-defining future stroke risk among pre-diabetics

Millions of pre-diabetic Americans may be at increased risk of future stroke, say researchers at the University of California, San Diego School of Medicine in a new meta-analysis of epidemiological studies, but the precise degree of that threat is confounded by differing medical definitions and factors that remain unknown or unmeasured.
“The immediate implication of our findings is that people with pre-diabetes should be aware they are at increased risk of stroke, and that this condition is frequently associated with one or more major risk factors for cardiovascular disease,” said Bruce Ovbiagele, MD, a professor of neurosciences at UC San Diego School of Medicine and the study's senior author. “Beyond that, there's a great need to further refine our understanding of that risk and how it's measured.”
Writing in the June 8 online edition of the British Medical Journal, Ovbiagele and an international team of colleagues reviewed 15 qualifying prospective cohort studies that looked at the association between pre-diabetes and stroke risk. The studies, published between 2004 and 2011, involved 760,925 participants.
Pre-diabetes occurs when blood glucose levels are consistently higher than normal, but not yet high enough to be diagnosed as diabetes. The condition is widespread in the United States: An estimated 35 percent of American adults – approximately 79 million people – are believed to be pre-diabetic, and thus at greater risk of developing full-blown type-2 diabetes, which afflicts roughly 26 million Americans. Diabetes is the seventh leading cause of death in the U.S., and a major risk factor for heart disease and stroke, the first and fourth leading causes of death.
People with pre-diabetes typically have the same risk factors for cardiovascular disease as people with type 2 diabetes – specifically, high blood pressure, high cholesterol levels and obesity – but the condition's effect on future stroke risk has not been established.
Ovbiagele and colleagues found that an association between future stroke risk and pre-diabetes depended upon the definition of the latter. To determine whether someone has pre-diabetes, blood glucose levels are typically measured after a 12-hour fast. According to the 1997 American Diabetes Association (ADA), a normal fasting glucose measurement ranges between 70.2 to 100 milligrams per deciliter (mg/dL). A level between 100 and 126 mg/dL is considered pre-diabetic. A level of 126 mg/dL or above is diabetic.
By the 1997 standard, the researchers found that pre-diabetics in the studies with a fasting glucose measurement of 110 to 125 mg/dL carried a 21 percent higher chance of suffering a future stroke. Heart disease and stroke account for roughly two-thirds of all deaths among people with diabetes.
In 2003, however, the ADA redefined the fasting glucose level for pre-diabetes to 100 to 125 mg/dL. Using this less stringent definition, the researchers found no increased stroke risk for pre-diabetics. Indeed, when they analyzed three studies that provided information on participants with fasting glucose levels of 100 to 109 mg/dL they found no increased risk of stroke.
Ovbiagele said the difference in the findings suggests there may be a “threshold effect” in the relationship between fasting glucose levels and future stroke risk. “Elevated risk may only begin at or above a fasting glucose level of 110 mg/dL,” he said.
Additional research is needed to determine the best definition predicting stroke risk among diabetics, Ovbiagele noted. It should include an assessment of more recent glycemic biomarkers, such as glycosylated hemoglobin, and be followed by randomized, controlled trials involving drugs and/or lifestyle modification to evaluate the effect of treatments on reducing the risk of future strokes.
“In the meantime, to avoid progression to diabetes or occurrence of strokes, clinicians should strongly consider recommending therapeutic lifestyle changes and maximizing the control of established stroke risk factors in their patients with pre-diabetes,” Ovbiagele said.
Co-authors of the study are Meng Lee, Chang Gung University College of Medicine, Chiayi, Taiwan; Jeffrey L. Saver and Sarah Song, University of California, Los Angeles; Heun-Sik Hong, Inje University, South Korea and Kuo-Hsuan Chang, Chang Gung University College of Medicine, Linkuo, Taiwan.
Funding, in part, came from Chang Gung Memorial Hospital and the National Institutes of Health (grants P50 NS044378 and U01 NS079179).
Media Contact
More Information:
http://www.ucsd.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Trotting robots reveal emergence of animal gait transitions
A four-legged robot trained with machine learning by EPFL researchers has learned to avoid falls by spontaneously switching between walking, trotting, and pronking – a milestone for roboticists as well…
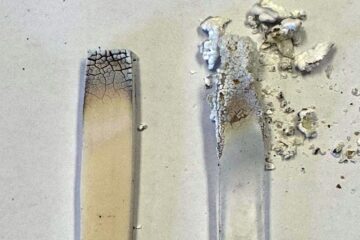
Innovation promises to prevent power pole-top fires
Engineers in Australia have found a new way to make power-pole insulators resistant to fire and electrical sparking, promising to prevent dangerous pole-top fires and reduce blackouts. Pole-top fires pose…
Possible alternative to antibiotics produced by bacteria
Antibacterial substance from staphylococci discovered with new mechanism of action against natural competitors. Many bacteria produce substances to gain an advantage over competitors in their highly competitive natural environment. Researchers…





















