Comparison of Venlafaxine and SSRIs in the Treatment of Depression

A new study published in the February 15th issue of Biological Psychiatry set out to compare two popular classes of antidepressants, the newer serotonin and norepinephrine reuptake inhibitors (SNRIs), like venlafaxine (Effexor), and the older selective serotonin reuptake inhibitors (SSRIs), like fluoxetine (Prozac) and citalopram (Celexa), to determine if one provides an overall greater benefit.
To do so, the authors performed a meta-analysis, by pooling the results of 34 double-blind randomized controlled trials that compared a single SNRI, venlafaxine, to other SSRIs. Dr. Charles Nemeroff, senior author on the paper, reports their findings: “Venlafaxine was superior to SSRIs in efficacy overall, and moreover, statistically superior to fluoxetine but not to paroxetine, sertraline or citalopram. Venlafaxine had a higher dropout rate due to adverse events.” These findings indicated a 5.9% advantage in remission rates for venlafaxine. The authors also report that the typical doctor would need to treat 17 patients to have a single patient benefit from being treated with venlafaxine rather than an SSRI.
Acknowledging the seemingly small advantage, John H. Krystal, M.D., Editor of Biological Psychiatry and affiliated with both Yale University School of Medicine and the VA Connecticut Healthcare System, comments that this article “highlights an advance that may have more importance for public health than for individual doctors and patients.” He explains this reasoning:
If the average doctor was actively treating 200 symptomatic depressed patients and switched all of them to venlafaxine from SSRI, only 12 patients would be predicted to benefit from the switch. This signal of benefit might be very hard for that doctor to detect. But imagine that the entire population of depressed patients in the United States, estimated to be 7.1% of the population or over 21 million people, received a treatment that was 5.9% more effective, then it is conceivable that more than 1 million people would respond to venlafaxine who would not have responded to an SSRI. This may be an example of where optimal use of existing medications may improve public health even when it might not make much difference for individual doctors and patients.
Thus, in the typical clinical practice this difference constitutes a barely detectable benefit, but this difference could be meaningful across the large population of depressed patients in the United States.
Media Contact
More Information:
http://www.elsevier.com/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Trotting robots reveal emergence of animal gait transitions
A four-legged robot trained with machine learning by EPFL researchers has learned to avoid falls by spontaneously switching between walking, trotting, and pronking – a milestone for roboticists as well…
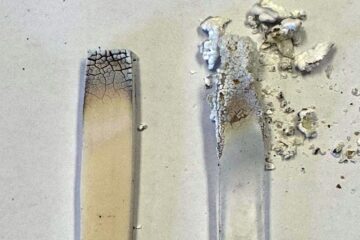
Innovation promises to prevent power pole-top fires
Engineers in Australia have found a new way to make power-pole insulators resistant to fire and electrical sparking, promising to prevent dangerous pole-top fires and reduce blackouts. Pole-top fires pose…
Possible alternative to antibiotics produced by bacteria
Antibacterial substance from staphylococci discovered with new mechanism of action against natural competitors. Many bacteria produce substances to gain an advantage over competitors in their highly competitive natural environment. Researchers…





















