Comparison of Venlafaxine and SSRIs in the Treatment of Depression

A new study published in the February 15th issue of Biological Psychiatry set out to compare two popular classes of antidepressants, the newer serotonin and norepinephrine reuptake inhibitors (SNRIs), like venlafaxine (Effexor), and the older selective serotonin reuptake inhibitors (SSRIs), like fluoxetine (Prozac) and citalopram (Celexa), to determine if one provides an overall greater benefit.
To do so, the authors performed a meta-analysis, by pooling the results of 34 double-blind randomized controlled trials that compared a single SNRI, venlafaxine, to other SSRIs. Dr. Charles Nemeroff, senior author on the paper, reports their findings: “Venlafaxine was superior to SSRIs in efficacy overall, and moreover, statistically superior to fluoxetine but not to paroxetine, sertraline or citalopram. Venlafaxine had a higher dropout rate due to adverse events.” These findings indicated a 5.9% advantage in remission rates for venlafaxine. The authors also report that the typical doctor would need to treat 17 patients to have a single patient benefit from being treated with venlafaxine rather than an SSRI.
Acknowledging the seemingly small advantage, John H. Krystal, M.D., Editor of Biological Psychiatry and affiliated with both Yale University School of Medicine and the VA Connecticut Healthcare System, comments that this article “highlights an advance that may have more importance for public health than for individual doctors and patients.” He explains this reasoning:
If the average doctor was actively treating 200 symptomatic depressed patients and switched all of them to venlafaxine from SSRI, only 12 patients would be predicted to benefit from the switch. This signal of benefit might be very hard for that doctor to detect. But imagine that the entire population of depressed patients in the United States, estimated to be 7.1% of the population or over 21 million people, received a treatment that was 5.9% more effective, then it is conceivable that more than 1 million people would respond to venlafaxine who would not have responded to an SSRI. This may be an example of where optimal use of existing medications may improve public health even when it might not make much difference for individual doctors and patients.
Thus, in the typical clinical practice this difference constitutes a barely detectable benefit, but this difference could be meaningful across the large population of depressed patients in the United States.
Media Contact
More Information:
http://www.elsevier.com/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
Silicon Carbide Innovation Alliance to drive industrial-scale semiconductor work
Known for its ability to withstand extreme environments and high voltages, silicon carbide (SiC) is a semiconducting material made up of silicon and carbon atoms arranged into crystals that is…
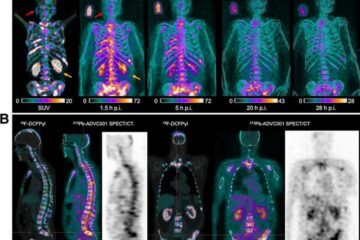
New SPECT/CT technique shows impressive biomarker identification
…offers increased access for prostate cancer patients. A novel SPECT/CT acquisition method can accurately detect radiopharmaceutical biodistribution in a convenient manner for prostate cancer patients, opening the door for more…

How 3D printers can give robots a soft touch
Soft skin coverings and touch sensors have emerged as a promising feature for robots that are both safer and more intuitive for human interaction, but they are expensive and difficult…





















