Carbon monoxide: Poison gas or anti-inflammatory drug?

Inhaling CO prevents transplant rejection in mice, say U-M scientists. Could become part of future treatment regimen for organ transplant patients
Could become part of future treatment regimen for organ transplant patients. Carbon monoxide, a poisonous gas that kills thousands of Americans every year, could turn out to be a life-saver for patients recovering from organ transplants, strokes or heart attacks, according to new research from the University of Michigan Cardiovascular Center.
In a recent study, U-M scientists found that inhaling small amounts of carbon monoxide for several weeks after transplant surgery prevented the development of a lethal inflammatory reaction in experimental mice receiving transplanted trachea, or windpipes.
If carbon monoxide therapy works as well in human patients as it does in mice, it could prevent an inflammatory response, called obliterative bronchiolitis, which develops in nearly 50 percent of all patients who receive a lung transplant from an unrelated donor. OB is the most common complication following a lung transplant in humans and the most deadly. It occurs when the patient’s immune system rejects the transplanted lung and sends an army of T cells to attack and destroy the foreign tissue.
“No one is sure exactly how it happens, but the small airways in the lung swell and become progressively smaller until the patient cannot breathe,” says David J. Pinsky, M.D., the J. Griswold Ruth, M.D. & Margery Hopkins Ruth Professor of Internal Medicine and chief of cardiovascular medicine in the U-M Medical School, who directed the research. “Currently, we have no effective treatments for OB. Unless the patient receives a new lung transplant, the outcome is generally fatal.”
Results of the U-M study were published July 18 in the most recent issue of the Journal of Experimental Medicine (JEM).
Pinsky’s research team focuses on the relationship between carbon monoxide and nitric oxide – two poisonous gases produced by different types of cells in the body. U-M research findings suggest that a patient’s chances of living or dying after a lung transplant depend, in large part, on the outcome of an internal power struggle between two enzymes that control cellular production of these gases.
“Hmox, or heme oxygenase enzyme, is responsible for the synthesis of carbon monoxide,” Pinsky explains. “It was first identified as a heat shock protein induced under stress conditions to help protect cells from damage. Hmox expression increases in human lung transplant patients with OB.
“Nitric oxide synthase, or iNOS, is the enzyme responsible for the synthesis of nitric oxide,” Pinsky adds. “When it’s expressed in endothelial cells in blood vessels, it causes them to dilate and relax. But when it’s expressed in epithelial cells in airways, it generates a flood of leukocytes that trigger an inflammatory response. Expression of iNOS also increases during lung transplant rejection.
“We think that Hmox and carbon monoxide are the body’s way of trying to limit tissue inflammation and injury induced by iNOS and nitric oxide during transplant rejection,” Pinsky says. “Our data show that localized CO production provides critical protection against the OB induced by iNOS expression. It’s a balancing mechanism. When Hmox expression goes up, it reduces iNOS expression and suppresses a key signaling pathway involved in the immune response.”
To test their hypothesis, U-M scientists studied two types of experimental mice – one group lacked the gene for the Hmox enzyme and were unable to synthesize carbon monoxide. Another group produced unusually high levels of Hmox and CO. When U-M scientists transplanted windpipes from one type of mouse into the other, genetic differences between the two strains of mice triggered transplant rejection, inflammation and significant narrowing of the airway in the transplant recipients.
But U-M scientists discovered they could rescue the mice by having them inhale CO-enriched air (100 ppm) for two weeks after transplantation, or by giving them a drug that induces high levels of Hmox expression.
“We found that naturally occurring levels of the Hmox enzyme were not high enough to prevent airway occlusion in mice after transplant,” says Hiroaki Harada, M.D., a U-M research fellow and co-first author of the study. “We had to either use drugs to boost Hmox expression in the mice or boost its end-product with prolonged inhalation of carbon monoxide.”
“Carbon monoxide is lethal at certain doses, but the animals tolerated the 100 ppm level for two weeks with no apparent problems,” Pinsky says. “In human terms, it’s equivalent to the amount you’d receive sitting in a traffic jam in Mexico City.”
The next step was to analyze the amount of Hmox enzyme expressed in white blood cells and in epithelial cells lining the grafted trachea. “We did this to determine the source of CO,” Pinsky says. “Was it coming from infiltrating immune cells from the host or from donor epithelial cells lining the graft? In order to prevent airway rejection, our results show that Hmox expression and generation of carbon monoxide must occur in grafted tissue cells.”
The researchers also found that while both inhaled and internally produced carbon monoxide had a positive effect on transplant airway inflammation and narrowing, inhaled nitric oxide had no effect and internally produced nitric oxide made the inflammatory reaction worse.
Pinsky’s research team previously published evidence for the therapeutic efficacy of CO inhalation in mice recovering from the type of cardiovascular injuries caused by blood clots to the lungs. Pinsky maintains that the balancing act between CO and NO is an important factor in transplant rejection after heart transplants and in recovery after other types of damage to the cardiovascular system.
Pinsky believes that carbon monoxide may one day be as common in the hospital ICU as inhaled nitric oxide is today, but cautions that a great deal of additional research will be required to resolve important questions of dosing and toxicity.
“The therapeutic window for carbon monoxide is very small,” he says. “Small amounts are good, but a little more will kill you. So dosage will always be a serious issue in any future therapies.”
Media Contact
More Information:
http://www.umich.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
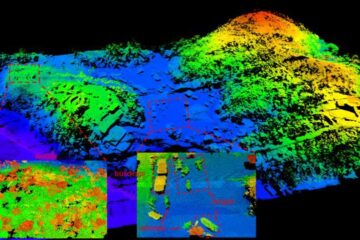
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















