Increased risk of ovarian cancer is linked to esNCI Press Officetrogen replacement therapy

Researchers from the National Cancer Institute (NCI) have found that women in a large study who used estrogen replacement therapy after menopause were at increased risk for ovarian cancer. The report was published in the July 17, 2002, issue of JAMA.* The scientists followed 44,241 women for approximately 20 years. Compared to postmenopausal women not using hormone replacement therapy, users of estrogen-only therapy had a 60 percent greater risk of developing ovarian cancer. The risk increased with length of estrogen use. The women, who were followed from 1979 to 1998, were former participants in the Breast Cancer Detection Demonstration Project, a mammography screening program conducted between 1973 and 1980.
“The main finding of our study was that postmenopausal women who used estrogen replacement therapy for 10 or more years were at significantly higher risk of developing ovarian cancer than women who never used hormone replacement therapy,” said James V. Lacey, Jr., Ph.D., lead author of the study from NCI’s Division of Cancer Epidemiology and Genetics.
The relative risk for 10 to 19 years of use was 1.8, which translates to an 80 percent higher risk than non-users, and increased to 3.2 (a 220 percent higher risk than non-users) for women who took estrogen for 20 or more years.
Estrogen is a natural hormone produced primarily by the ovaries. After menopause, the ovaries produce lower levels of the hormones estrogen and progesterone. By the time natural menopause is complete – usually between ages 45 and 55 – hormone output decreases significantly.
As early as the 1940s, women began using estrogens in high doses to counteract some of the short-term discomforts of menopause (hot flashes, vaginal drying and thinning, and urinary tract incontinence and infections).
However, after it became clear in the 1970s that women who took estrogen alone had a six to eight times higher risk of developing endometrial cancer (cancer of the lining of the uterus), doctors began prescribing progestin along with much lower doses of estrogen. Progestin is a synthetic form of the natural hormone progesterone. The addition of progestin to estrogen therapy reduces the increased risk of endometrial cancer associated with using estrogen alone. As a result, it has become increasingly common to prescribe estrogen-progestin therapy for women who have not had a hysterectomy.
In addition to studying the effect of estrogen use alone, Lacey and his colleagues looked at whether women using estrogen-progestin therapy were more likely to develop ovarian cancer. No increased risk was found. Lacey commented, “Even though our data showed that women who took estrogen combined with progestin were not at increased risk for ovarian cancer, only a few women in our study who developed ovarian cancer had used estrogen-progestin therapy for more than four years. So, at this point, there simply aren’t enough data to say whether taking the combined therapy has any effect on ovarian cancer.”
Past studies suggested that postmenopausal hormone treatments might be effective in preventing or reducing some of the negative long-term effects of aging, such as heart disease and osteoporosis. However, the results from a large multi-center clinical trial, also published in the July 17 issue of JAMA (JAMA 2002;288:321-333), showed increases in breast cancer, coronary heart disease, stroke, and blood clots in the lungs and legs for women on estrogen-progestin therapy for an average of 5.2 years.
The trial, part of the Women’s Health Initiative (WHI), also found fewer cases of hip fractures and colon cancer among women taking the combined therapy. However, because overall the harm was greater than the benefit, the trial was stopped last week, three years ahead of schedule. The WHI randomized trial for estrogen alone in women who have had their uterus removed is continuing.
Lacey emphasized the complexity of weighing the various risks and benefits of hormone use. “Because hormone therapy may influence so many conditions that affect women after menopause – cardiovascular disease, osteoporosis, breast cancer, uterine cancer, gallbladder disease, blood clots, and now potentially ovarian cancer – we should no longer think of a woman basing her decision to use hormones on the potential risk of just one condition. Women should continue to talk to their health care providers about whether hormones might be right for them.”
Previous studies looking at the effect of postmenopausal hormones on ovarian cancer risk have been inconsistent. Some reported increased risk with estrogen use while others reported either no effect or a protective one. Most of these earlier studies were relatively small and limited by incomplete information about ovarian cancer risk factors.
Two recent large studies found a link between hormone use and ovarian cancer. A large prospective study published last year (JAMA 2001;285:1460-1465) showed that postmenopausal estrogen use for 10 or more years was associated with increased risk of ovarian cancer mortality, and a recent Swedish study (J. Natl. Cancer Inst. 2002;94:497-504) reported that estrogen use alone and estrogen-progestin used sequentially (progestin used on average 10 days/month) may be associated with an increased risk for ovarian cancer. In contrast, estrogen-progestin used continuously (progestin used on average 28 days/month) seemed to confer no increased ovarian cancer risk.
Lacey said that some of the unknowns concerning hormone use and ovarian cancer include the following:
- Duration vs. dose of estrogen therapy It is not clear from this study whether the increased risk with estrogen use is due to higher doses of estrogen, longer duration of estrogen use, or both dose and duration. It is also not clear whether long-term use of lower-dose estrogen is associated with ovarian cancer.
- Duration of estrogen-progestin therapy Most women in this study were on the combined therapy for less than four years, so more data will be needed to determine whether estrogen-progestin use increases risk. The effect of long-term use of estrogen-progestin therapy is not known.
- The type of estrogen-progestin regimen The continuous regimen involves taking both hormones simultaneously throughout the month. The sequential regimen, on the other hand, involves taking estrogen every day, and progestin for 10 to 14 days each month.
- Use of more than one type of hormone replacement therapy For instance, after taking estrogen alone, some women changed to a combined regimen after reports of increased endometrial cancer risk with estrogen alone. More data are needed to analyze the effect of switching from one regimen to another.
- The form of estrogen administration Most studies have analyzed the use of estrogens in pill form, but it can also be administered by patches, shots, and creams.
Every year, about 23,000 U.S. women are diagnosed with ovarian cancer and 14,000 women die from the disease. A woman’s lifetime risk of developing ovarian cancer is 1.7 percent. This means that in a group of 100 women followed from birth to age 85, fewer than two would get ovarian cancer. In comparison, about 13 women would get breast cancer (lifetime risk is 13.3 percent), fewer than three women would develop uterine cancer (lifetime risk is 2.7 percent), and between 16 and 32 women would develop osteoporosis.
An estimated 40 million U.S. women will experience menopause during the next 20 years, and women today are living approximately one-third of their life after menopause.
Anywhere from 20 percent to 45 percent of U.S. women take some form of hormone therapy between the ages of 50 and 75. According to industry estimates, about 8 million U.S. women use estrogen alone and about 6 million U.S. women use estrogen-progestin therapy. About 20 percent of hormone users continue for more than five years.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
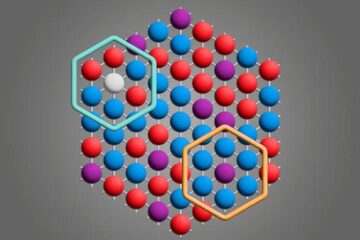
Microscopic basis of a new form of quantum magnetism
Not all magnets are the same. When we think of magnetism, we often think of magnets that stick to a refrigerator’s door. For these types of magnets, the electronic interactions…

An epigenome editing toolkit to dissect the mechanisms of gene regulation
A study from the Hackett group at EMBL Rome led to the development of a powerful epigenetic editing technology, which unlocks the ability to precisely program chromatin modifications. Understanding how…
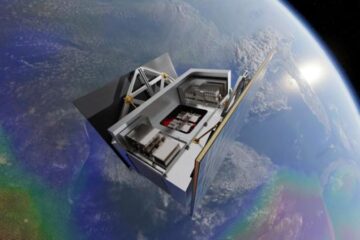
NASA selects UF mission to better track the Earth’s water and ice
NASA has selected a team of University of Florida aerospace engineers to pursue a groundbreaking $12 million mission aimed at improving the way we track changes in Earth’s structures, such…





















