Penn study points to novel way to improve outcomes from umbilical cord blood transplants

A new method to boost the number of immune cells in umbilical cord blood prior to cord blood transplants for cancer patients appears to lead to a quicker rebuilding of a new immune system in the patient's body than with a conventional cord blood transplant procedure, according to new research from the Perelman School of Medicine at the University of Pennsylvania that will be presented today at the 53rd American Society of Hematology Annual Meeting. The technique also paves the way for the development of a way to provide these transplant patients with a salvage therapy from the same donor if their cancer returns.
“Umbilical cord blood is a potential cancer therapy that is thrown away every day,” said lead author Elizabeth Hexner, MD, an assistant professor in the division of Hematology-Oncology in Penn's Abramson Cancer Center. “Our findings point to a promising method to make better use of scarce cord blood resources available through public banks, which offer the only transplant option for patients who have no suitably matched blood or bone marrow donor prospects.”
Though cord blood has a larger number of stem cells by volume than blood or marrow from living donors, the actual amount of blood available per cord is smaller – containing about one tenth the number of cells collected from living donors. That deficit typically leads to a slower rebuilding of a sick patient's new immune system following transplant, leaving patients vulnerable to severe, even life-threatening infections. On the other hand, because immune cells in cord blood are less developed and have not been fully “educated” to attack perceived invaders in the body, patients who undergo cord blood transplants are less likely to suffer graft-versus-host disease (GVHD) — a common, dangerous complication in which the new cells assault healthy organs like the liver and skin — doctors say that improvements to the transplant procedure hold great potential.
The procedure used in the Penn trial, involving four patients, began with cord blood donations that had been separated into two parts – typically an 80 percent fraction and a 20 percent fraction – prior to freezing. Then, the team thawed the smaller fraction two weeks prior to transplant, activated and grew the number of donated T cells — which are a key driver for the process that recovers transplant patients' immune system and play a role in fighting infections — using the co-stimulatory compounds CD3 and CD28 in Penn's Clinical Cell and Vaccine Production Facility. Following a chemotherapy and radiation regimen to destroy patients' remaining cancer cells and the administration of immunosuppression drugs to prevent rejection of the donor cells, patients then received the thawed, larger fraction of the cord blood first (a standard, single cord blood transplant). An infusion of the newly activated and expanded T cells followed, with a portion of those cells being reserved and frozen for potential future use as immunotherapy in the event of a cancer relapse or transplant failure.
“Donor lymphocyte infusions (DLI) are frequently given to patients who need them following stem cell transplants from living donors, but until now, we have been unable to offer this therapy to cord blood transplant patients because the source of their cells is used up at the time of transplant,” Hexner says. “Our results show that we are able to grow sufficient numbers of T cells to be available both for that use as well as to buoy the number of cells that patients receive during the transplant itself, which seems to have helped their immune systems come back online more quickly than is typically seen in umbilical cord blood transplants.”
Three of the patients enrolled on the study experienced relatively early neutrophil engraftment – the point at which these critical infection fighting cells in our body reach 500 per microliter. This milestone is important because above this threshold, the risk of life-threatening infections is drastically lower. For these three patients, engraftment was achieved on days 12, 20, and 17 post-transplant. This was approximately half the time this process has historically taken with this type of transplant, substantially narrowing the window in which patients have the greatest risk of death from transplant complications. Research has shown that using two cords per transplant can also speed this process, but that tactic also doubles the cost of the procedure, to more than $60,000. The fourth trial patient's umbilical cord blood graft failed, and they were subsequently treated with another stem cell transplant. There were no infusion-related adverse events observed during the trial, and three of the four expansion samples yielded enough cells for future immunotherapeutic DLI use. Next, the team hopes to test the optimal expanded T cell dose necessary for speeding the process of immune recovery and develop a method to perform DLI after transplant.
Though the new research paves the way for improvements in the use of existing cord blood resources to improve transplant outcomes, the Penn team says their work also sheds light on the need to buoy the number of public cord blood banks through which new parents can opt to donate their newborns' cord blood for use treating sick patients. Commercial, private cord blood banks have proliferated in the United States in recent years, despite a lack of evidence proving the utility of this so-called “biological insurance” and statements from the American Academy of Pediatrics and other groups discouraging new parents from paying for the service.
Since cord blood stored in public banks is already frozen and awaiting use, it offers a less labor intensive, quicker way to match patients for transplant than the two to three month timeframe for locating and obtaining cells from a matching unrelated donor through the National Marrow Donor Program. Blood stored in private banks, however, is not available for treatment of unrelated donors for whom a living blood or marrow donor cannot be located.
“In many parts of the country, even families who want to donate their infant's cord blood for care of unrelated sick patients are not able to do so because no public bank exists in their area,” Hexner says. “Greater investment in public banks and more opportunities for parents to donate to these banks are a necessary component of improving care for patients with blood cancers.”
The trial was funded by the Leukemia and Lymphoma Society, the National Institutes of Health (K23 NHLBI K23-HL-093366), and from the Abramson Cancer Center's Alan Steinberg Scholars in Cancer Research Fund.
The study will be presented from 6 PM to 8 PM PST in Hall GH of the San Diego Convention Center.
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $4 billion enterprise.
Penn's Perelman School of Medicine is currently ranked #2 in U.S. News & World Report's survey of research-oriented medical schools and among the top 10 schools for primary care. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $507.6 million awarded in the 2010 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania — recognized as one of the nation's top 10 hospitals by U.S. News & World Report; Penn Presbyterian Medical Center; and Pennsylvania Hospital – the nation's first hospital, founded in 1751. Penn Medicine also includes additional patient care facilities and services throughout the Philadelphia region.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2010, Penn Medicine provided $788 million to benefit our community.
Media Contact
More Information:
http://www.uphs.upenn.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
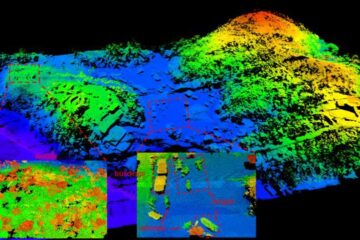
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















