Penn Researchers attach Lyme disease antibodies to nanotubes, paving way for diagnostic device

Existing tests assess the presence of antibodies against bacterial proteins, which take weeks to form after the initial infection and persist after the infection is gone. Now, a nanotechnology-inspired technique developed by researchers at the University of Pennsylvania may lead to diagnostics that can detect the organism itself.
The study was led by professor A. T. Charlie Johnson of the Department of Physics and Astronomy in Penn's School of Arts and Sciences along with graduate student Mitchell Lerner, undergraduate researcher Jennifer Dailey and postdoctoral fellow Brett R. Goldsmith, all of Physics. They collaborated with Dustin Brisson, an assistant professor of biology who provided the team with expertise on the bacterium.
Their research was published in the journal Biosensors and Bioelectronics.
“When you're initially infected with the Lyme disease bacterium, you don't develop antibodies for many days to a few weeks,” Johnson said. “Many people see their physician before antibodies develop, leading to negative serological test results. And after an initial infection, you're still going to have these antibodies, so using these serological diagnostics won't make it clear if you're still infected or not after you've been treated with antibiotics.”
The research team's idea was to flip the process around, using laboratory-produced antibodies to detect the presence of proteins from the organism. This is an extension of previous work Johnson's lab has done connecting other biological structures, such as olfactory receptors and DNA, to carbon nanotube-based devices.
Carbon nanotubes, rolled-up lattices of carbon atoms, are highly conductive and sensitive to electrical charge, making them promising components of nanoscale electronic devices. By attaching different biological structures to the exteriors of the nanotubes, they can function as highly specific biosensors. When the attached structure binds to a molecule, that molecule's charge can affect the electrical conduction of the nanotube, which can be part of an electrical circuit like a wire. Such a device can therefore provide an electronic read-out of the presence, or even concentration, of a particular molecule.
To get the electrical signal out of these nanotubes, the team first turned them into transistor devices.
“We first grow these nanotubes on what amounts to a large chip using a vapor deposition method, then make electrical connections essentially at random,” Johnson said. “We then break up the chip and test all of the individual nanotube transistors to see which work the best.”
In their recent experiment, Johnson's team attached antibodies that naturally develop in most animals that are infected with the Lyme disease bacterium to these nanotube transistors. These antibodies naturally bind to an antigen, in this case, a protein in the Lyme bacterium, as part of the body's immune response.
“We have a chemical process that lets us connect any protein to carbon nanotubes. Nanotubes are very stable, so we have a very reactive compound that binds to the nanotube and also has a carboxylic acid group on the other end. For biochemists, getting any kind of protein to bind to a carboxylic acid group is just child's play at this point, and we have worked with them to learn how to perform this chemistry on the side wall of nanotubes. “
After using atomic-force microscopy to show that antibodies had indeed bound to the exteriors of their nanotube transistors, the researchers tested them electrically to get a baseline reading. They then put the nanotubes in solutions that contained different concentrations of the target Lyme bacteria protein.
“When we wash away the solution and test the nanotube transistors again, the change in what we measure tells us that how much of the antigen has bound,” Johnson said. “And we see the relationship we expect to see, in that the more antigen there was in the solution, the bigger the change in the signal.”
The smallest concentration the nanotube devices could detect was four nanograms of protein per milliliter of solution.
“This sensitivity is more than sufficient to detect the Lyme disease bacterium in the blood of recently-infected patients and may be sufficient to detect the bacterium in fluids of patients that have received inadequate treatment,” Brisson said.
“We really want the protein we are looking to detect to bind as close to the nanotube as possible, as that is what increases the strength of the electrical signal,” Johnson said. “Developing a smaller, minimal version of the antibody — what we call a single chain variable fragment — would be a next step.
“Based on our previous work with single chain variable fragments of other antibodies, this would probably make such a device about a thousand times more sensitive.”
The researchers suggested that, given the flexibility of their technique for attaching different biological structure, eventual diagnostic tools could incorporate multiple antibodies, each detecting a different protein from the Lyme bacterium. Such a setup would improve accuracy and cut down on the possibility of false-positive diagnoses.
“If we were to do this type of test on a person's blood now, however, we would say the person has the disease,” Johnson said. “The first thought is that if you detect any protein coming from the Lyme organism in your blood, you are infected and should get treatment right away.”
This research was supported by the Department of Defense U.S. Army Medical Research and Materiel Command, the National Institutes of Health, Penn's Nano/Bio Interface Center, the National Science Foundation and Penn's Laboratory for Research on the Structure of Matter.
Media Contact
More Information:
http://www.upenn.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
A universal framework for spatial biology
SpatialData is a freely accessible tool to unify and integrate data from different omics technologies accounting for spatial information, which can provide holistic insights into health and disease. Biological processes…
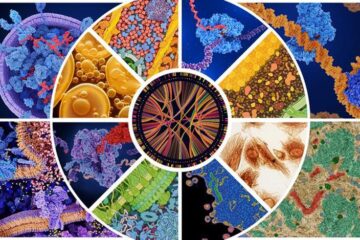
How complex biological processes arise
A $20 million grant from the U.S. National Science Foundation (NSF) will support the establishment and operation of the National Synthesis Center for Emergence in the Molecular and Cellular Sciences (NCEMS) at…
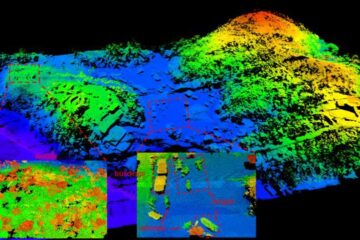
Airborne single-photon lidar system achieves high-resolution 3D imaging
Compact, low-power system opens doors for photon-efficient drone and satellite-based environmental monitoring and mapping. Researchers have developed a compact and lightweight single-photon airborne lidar system that can acquire high-resolution 3D…





















