Bone marrow cells used in bladder regeneration

The Northwestern Medicine® research, which will be published February 18 in the Proceedings of the National Academy of Sciences by lead author Arun K. Sharma, research assistant professor in urology at Northwestern University Feinberg School of Medicine and colleagues, is an alternative to contemporary tissue-engineering strategies. The bone marrow cells are being used to recreate the organ's smooth muscle, vasculature, and nerve tissue.
“We are manipulating a person's own disease-free cells for bladder tissue reformation,” said Sharma, a member of the Institute for BioNanotechnology in Medicine and the Ann & Robert H. Lurie Children's Hospital of Chicago Research Center. “We have used the spina bifida patient population as a proof of concept model because those patients typically have bladder dysfunction. However, this regeneration approach could be used for people suffering from a variety of bladder issues where the bone marrow microenvironment is deemed normal.”
In end-stage neurogenic bladder disease – an illness often associated with spinal cord diseases like spina bifida – the nerves which carry messages between the bladder and the brain do not work properly, causing an inability to pass urine. The most common surgical option, augmentation cystoplasty, involves placing a “patch” derived from an individual's bowel over a part of the diseased organ in order to increase its size. The current “gold standard,” the procedure remains problematic because the bowel tissue introduces long-term complications like the development of electrolyte imbalance and bladder cancer.
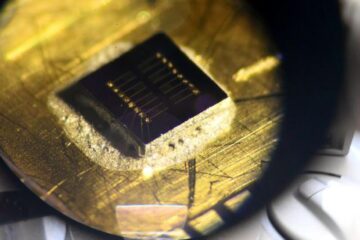
Because Sharma's procedure does not use bowel tissue, it offers the benefits of augmentation without the association of long-term risks. His technique combines stem and progenitor cells from a patient's bone marrow with a synthetic scaffold created in the lab of Guillermo Ameer, ScD, professor of biomedical engineering at McCormick School of Engineering and Applied Science and of surgery at Feinberg. The scaffold takes the place of the traditional patch.
“We decided to use material that has the ability to be tailored to simulate mechanical properties of the bladder,” said Sharma, director of pediatric urological regenerative medicine at Lurie Children's. “Using the elastomer created by Dr. Ameer and the bone marrow stem and progenitor cells, I believe that we have developed a technique that can potentially be used in lieu of current bladder augmentation procedures. However, further study is needed.”
Sharma's initial research was supported in part by an Excellence in Academic Medicine grant funded by the Illinois Department of Healthcare and Family Services.
Media Contact
More Information:
http://www.northwestern.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Sea slugs inspire highly stretchable biomedical sensor
USC Viterbi School of Engineering researcher Hangbo Zhao presents findings on highly stretchable and customizable microneedles for application in fields including neuroscience, tissue engineering, and wearable bioelectronics. The revolution in…

Twisting and binding matter waves with photons in a cavity
Precisely measuring the energy states of individual atoms has been a historical challenge for physicists due to atomic recoil. When an atom interacts with a photon, the atom “recoils” in…
Nanotubes, nanoparticles, and antibodies detect tiny amounts of fentanyl
New sensor is six orders of magnitude more sensitive than the next best thing. A research team at Pitt led by Alexander Star, a chemistry professor in the Kenneth P. Dietrich…





















