Hurdles ahead for health care reform primary care model, U-M study shows

Provisions of new federal health care reforms will move the country toward a primary care medical home for patients, but the nation may not have enough primary care doctors to handle the workload, according to a study by the University of Michigan Health System.
Still, the concept of shifting patients to a medical home could save time and money and allow specialists to focus on complex patient care, according to the study published online ahead of print in the journal Medical Care.
“I don’t think anyone would question that there are too few primary care physicians,” says study lead author John M. Hollingsworth, M.D., M.S., an assistant professor of urology at the U-M Medical School. “The issue that came up in our study pertains to the role of specialist physicians in the new ‘medical neighborhood.’
“Policymakers need to consider the scope and magnitude of care for which specialists are currently responsible in these delivery system reforms,” he says.
Specialists spend a significant amount of time handling routine follow-up care for patients with chronic conditions that might be more cost-effectively delegated to primary care physicians.
But redistributing half of that workload could require either thousands of new primary care doctors or an extra three weeks of work a year from the primary care physicians in the current workforce, the study found.
U-M researchers examined the implications of redistributing the chronic disease care workload between specialists and primary care physicians under a patient-centered medical home model of care.
Known as PCMH, the model places an emphasis of having primary care doctors coordinate and quarterback their patients’ medical care across multiple locations and settings; creating cost-savings by delegating less complex aspects of care; and shifting from an emphasis on volume under the fee-for-service model, to one that rewards the quality of the outcomes using performance measures.
The approach was an important part of the recent health care reform legislation and is becoming an increasingly popular solution to the current fragmentation and inefficiencies in the health care delivery system, the authors say.
According to the study, specialists spend a significant amount of time each year – more than 650,000 work weeks collectively – on routine follow-up care for patients with common chronic conditions, such as asthma, diabetes and low back pain.
Delegating a proportion of this care has the potential to create system-wide efficiencies by freeing up specialists to concentrate more on new patients and those with complex conditions.
“The cumulative time spent by specialists on routine chronic care is not trivial,” says the study’s senior author David C. Miller, M.D., M.P.H., an assistant professor of urology at the U-M Medical School.
“As a urologic oncologist, I take care of many cancer survivors. With a detailed care plan constructed by the treating oncologist, much of the follow-up care for these patients could potentially be assumed by a primary care physician-directed medical home, with appropriate referral back to me if problems or questions arise.
“This approach may have benefits for patients in terms of improving both coordination and access to care,” Miller says.
Miller and several other study authors are affiliated with the Veteran’s Affairs Ann Arbor Health Care System. The VA is one of two major federal departments that are moving toward implementing patient-center medical home reforms.
The medical home model also offers other potential benefits including less fragmentation of care, in which a patient’s physicians aren’t aware of what the others are doing; minimization of redundant tests and services; and more prestige and pay for primary care physicians, which may help entice more medical student to enter general medicine.
Methods:The study analyzed data from the 2007 National Ambulatory Medical Care Survey for seven chronic conditions: chronic obstructive pulmonary disease/asthma, low back pain, diabetes mellitus, coronary artery disease/congestive heart failure, chronic kidney disease and depression. Researchers examined the time specialists spent with patients for direct and indirect follow-up care for those conditions.
Additional U-M Authors:Sanjay Saint, M.D., M.P.H.; Rodney A. Hayward, M.D.; Mary A. M. Rogers, Ph.D.; Lingling Zhang, M.A., all also of the Veteran’s Affairs Ann Arbor Health Care System.
Funding:The Robert Wood Johnson Foundation Clinical Scholars Program and the Agency for Healthcare Research and Quality.
Resources:
Patient Centered Primary Care Collaborative, www.pcpcc.net
American College of Physicians, www.acponline.org/running_practice/pcmh
Media Contact
More Information:
http://www.umich.eduAll latest news from the category: Studies and Analyses
innovations-report maintains a wealth of in-depth studies and analyses from a variety of subject areas including business and finance, medicine and pharmacology, ecology and the environment, energy, communications and media, transportation, work, family and leisure.
Newest articles

Trotting robots reveal emergence of animal gait transitions
A four-legged robot trained with machine learning by EPFL researchers has learned to avoid falls by spontaneously switching between walking, trotting, and pronking – a milestone for roboticists as well…
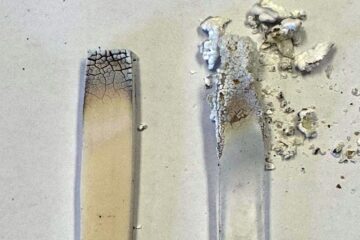
Innovation promises to prevent power pole-top fires
Engineers in Australia have found a new way to make power-pole insulators resistant to fire and electrical sparking, promising to prevent dangerous pole-top fires and reduce blackouts. Pole-top fires pose…
Possible alternative to antibiotics produced by bacteria
Antibacterial substance from staphylococci discovered with new mechanism of action against natural competitors. Many bacteria produce substances to gain an advantage over competitors in their highly competitive natural environment. Researchers…





















