While some immune cells aim to fight cancer, others hold them in check

Many cancer patients generate immune cells capable of specifically attacking their tumors, but the cells rarely do, in fact, target a patient’s cancer. What prevents these potentially helpful cells from taking action? And is there anything that might be done to unleash them?
The attack cells – known as cytolytic T cells – are prevented from acting by a second set of immune cells called regulatory T cells, according to a new study from investigators at The Wistar Institute. The research also shows that the regulatory T cells communicate their message of restraint to the cytolytic T cells at a distance, via a messenger chemical called TGF-beta. A report on the study appears in the September 15 issue of Cancer Research.
Previous work has focused on ways to stimulate the cytolytic T cells to act, but the new study suggests that other approaches to bringing them into the battle against cancer might be more effective. For example, a drug that inactivates the regulatory T cells or that blocks the TGF-beta chemical message they send might free the cytolytic T cells to attack a patient’s tumor.
“We’ve known for some time that cancer patients can generate T cells able to attack their tumors,” says immunologist Dorothee Herlyn, D.V.M., D.Sc., a professor at The Wistar Institute and senior author on Cancer Research study. “What we discovered in this study is that those patients also produce negatively regulating cells at the same time that keep the attacking T cells in check. The existence of these regulatory cells may help explain how tumors are able to evade the immune system. They also represent a new starting point for thinking about novel anti-cancer treatments.”
The current study evolved somewhat by chance. Using cells from a human colorectal cancer patient, Herlyn’s laboratory team was working to identify T cells with cancer-fighting capabilities and isolate them from other types of immune cells. At one point, one of her coworkers suggested combining different groups of isolated cell types to look for interactions between them.
“We put these two different types of immune cell together, one of which killed cancer cells in culture, the other of which did not,” Herlyn recalls. “When we did, we were stunned to see that the one that had previously killed cancer cells no longer did so.”
Adequately explaining the mechanisms underlying that observation required several years of additional study, she says.
Media Contact
More Information:
http://www.wistar.upenn.edu/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Webb captures top of iconic horsehead nebula in unprecedented detail
NASA’s James Webb Space Telescope has captured the sharpest infrared images to date of a zoomed-in portion of one of the most distinctive objects in our skies, the Horsehead Nebula….
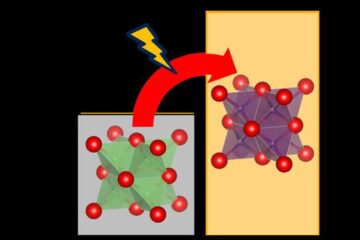
Cost-effective, high-capacity, and cyclable lithium-ion battery cathodes
Charge-recharge cycling of lithium-superrich iron oxide, a cost-effective and high-capacity cathode for new-generation lithium-ion batteries, can be greatly improved by doping with readily available mineral elements. The energy capacity and…
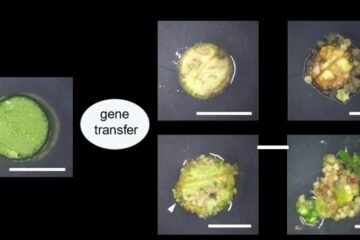
Novel genetic plant regeneration approach
…without the application of phytohormones. Researchers develop a novel plant regeneration approach by modulating the expression of genes that control plant cell differentiation. For ages now, plants have been the…





















