Trauma patients protected from worse outcomes associated with so-called 'weekend effect'

Patients who've been hurt in car or bike crashes, been shot or stabbed, or suffered other injuries are more likely to live if they arrive at the hospital on the weekend than during the week, according to new University of Pennsylvania School of Medicine research published in the March 21 issue of Archives of Surgery.
The findings, which also showed that trauma patients who present to the hospital on weeknights are no more likely to die than those who presented during the day, contrast with previous studies showing a so-called “weekend effect” in which patients with emergent illnesses such as heart attacks and strokes fare worse when they're hospitalized at night or on weekends.
The authors say the trauma system's unique organization and staffing appears to serve as a built-in protection for these critically injured patients, and may provide a roadmap for ongoing efforts to restructure and better coordinate U.S. emergency care, which needs to provide optimal care day or night.
“Whether patients have an emergent illness or a severe injury, the common denominator is time. Patients must rely on the system to quickly get them to the place that's best prepared to save their lives,” says lead author Brendan G. Carr, MD, MS, an assistant professor in the departments of Emergency Medicine and Biostatistics and Epidemiology. “Trauma systems have been designed to maximize rapid access to trauma care, and our results show that the system also offers special protection for patients injured during periods that are known to be connected to worse outcomes among patients with time-sensitive illnesses.”
Using data provided by the Pennsylvania Trauma Systems Foundation, Carr and senior author Douglas J. Wiebe, PhD, an assistant professor of Biostatistics and Epidemiology, studied 90,461 patients who were treated from 2004 to 2008 at Pennsylvania's 32 accredited trauma centers. About a quarter of the patients presented to the hospital on weeknights (defined as 6 p.m. to 9 a.m. Monday through Friday) and about 40 percent arrived on weekends (6 p.m. Friday to 9 a.m. on Monday). In addition to the survival-related findings, neither the weekend or night patient group experienced delays for crucial brain or abdominal surgeries often required for trauma patients, compared to weekday patients.
Across the United States, trauma patients are cared for by a regionalized system dictating that they be brought to facilities that meet strict requirements for round-the-clock staffing and capabilities for emergency medicine, radiology, surgery, and post-operative intensive care. Unlike most other medical and surgical specialties – in which staffing and resources vary on nights and weekends – trauma centers like the Hospital of the University of Pennsylvania are required to have these resources immediately available 24 hours a day, seven days a week, 365 days a year.
In addition to the constant presence of specialty staff, the authors suggest that the greater odds of survival on weekends uncovered in the study may be influenced by hospital scheduling factors. Since elective surgeries are typically not performed over the weekend, there is less competition for practitioners' time, operating rooms, blood bank, pharmacy and other hospital resources – perhaps leading to expedited care for trauma patients during those times.
Despite the indication that trauma patients may, overall, be safer during off hours, the findings revealed that both weeknight and weekend presentation was associated with longer intensive care unit stays, and those who came to the hospital on weeknights were more likely to have a longer hospital stay overall than those who were admitted on a weekday. The authors suggest this may also be due to hospital factors not entirely related to the patient's condition, including greater bed availability because few elective admissions and surgeries occur on weekends.
Although the findings focus on injury outcomes and don't directly address care for other time sensitive conditions, the authors believe they offer solutions for improving care for all emergency patients. “There are complex questions that need to be addressed about our expectations around emergency care,” Carr says. “It is unrealistic to think that all hospitals can be fully staffed to provide optimal care for all time-sensitive conditions all of the time, so our challenge is to develop an integrated system of emergency care for unplanned – but inevitable – critical illness. The trauma system has a plan of care in place long before we ever need it, and it offers many lessons for the remainder of emergency care.”
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the University of Pennsylvania School of Medicine (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $4 billion enterprise.
Penn's School of Medicine is currently ranked #2 in U.S. News & World Report's survey of research-oriented medical schools and among the top 10 schools for primary care. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $507.6 million awarded in the 2010 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania — recognized as one of the nation's top 10 hospitals by U.S. News & World Report; Penn Presbyterian Medical Center; and Pennsylvania Hospital – the nation's first hospital, founded in 1751. Penn Medicine also includes additional patient care facilities and services throughout the Philadelphia region.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2010, Penn Medicine provided $788 million to benefit our community.
Media Contact
More Information:
http://www.uphs.upenn.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
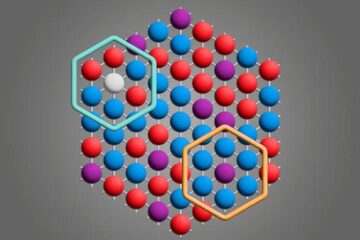
Microscopic basis of a new form of quantum magnetism
Not all magnets are the same. When we think of magnetism, we often think of magnets that stick to a refrigerator’s door. For these types of magnets, the electronic interactions…

An epigenome editing toolkit to dissect the mechanisms of gene regulation
A study from the Hackett group at EMBL Rome led to the development of a powerful epigenetic editing technology, which unlocks the ability to precisely program chromatin modifications. Understanding how…
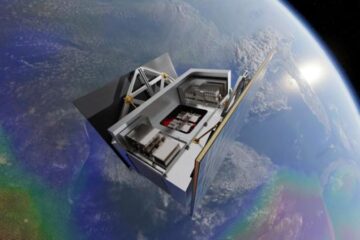
NASA selects UF mission to better track the Earth’s water and ice
NASA has selected a team of University of Florida aerospace engineers to pursue a groundbreaking $12 million mission aimed at improving the way we track changes in Earth’s structures, such…





















