Sun-damaged skin does not improve with estrogen treatments

Treating the skin with estrogen can stimulate collagen production—which improves the appearance of the skin—in areas not typically exposed to the sun, according to new research from the University of Michigan Health System.
But in sun-damaged skin, the same treatment does not increase collagen production, the study found. The findings elucidate why it is so difficult to reverse the effects of sun damage on the skin, says lead author Laure Rittie, Ph.D., research investigator in the U-M Department of Dermatology.
“Frankly, we were very surprised to find that stimulation of collagen production by topical estrogen treatment was restricted to skin not chronically exposed to sunlight. These results suggest that sun exposure alters the ability of skin to respond to topical estrogen, and point out how difficult it is to repair photoaged skin,” Rittie says. The study appears in the new issue of the Archives of Dermatology.
Seventy seniors—40 post-menopausal women and 30 men—participated in the study. Researchers analyzed biopsies of skin taken from the patients' hips, and either forearm or face, before treatment began and after it ended two weeks later.
The study participants all had photoaged skin—that is, sun-damaged skin that appears dry, with coarse wrinkles and uneven pigmentation.
Participants were treated topically with the estrogen medication called estradiol. They were given doses of 0.01 percent, 0.1 percent, 1 percent or 2.5 percent, or a vehicle that contained no estradiol.
Estradiol was found to increase collagen levels in women's hip skin more than threefold, on average, compared with the inactive medication. This included procollagen I and III mRNA levels. In men, the collagen levels increased by a factor of about 1.7 on average. The improvements were higher when the doses of estradiol were higher.
In contrast, collagen levels in the photoaged skin on the forearm and face did not improve significantly with treatment, no matter the dosage of estradiol.
Authors: Authors in addition to Rittié, were: Sewon Kang, M.D., professor of dermatology; John J. Voorhees, M.D., the Duncan and Ella Poth Distinguished Professor and chair, Department of Dermatology; and Gary J. Fisher, Ph.D.,Harry Helfman Professor of Molecular Dermatology.
Funding: A grant from Pfizer Inc. supported the research in part.
Disclosure: Voorhees was a consultant for Pfizer Inc. and received consulting payments.
Reference: Archives of Dermatology, Vol. 144, No. 9, Sept. 2008.
Media Contact
More Information:
http://www.umich.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
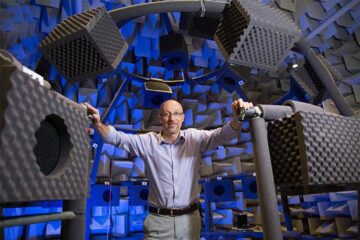
Why getting in touch with our ‘gerbil brain’ could help machines listen better
Macquarie University researchers have debunked a 75-year-old theory about how humans determine where sounds are coming from, and it could unlock the secret to creating a next generation of more…
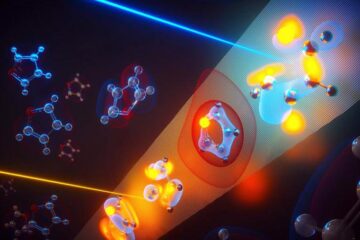
Attosecond core-level spectroscopy reveals real-time molecular dynamics
Chemical reactions are complex mechanisms. Many different dynamical processes are involved, affecting both the electrons and the nucleus of the present atoms. Very often the strongly coupled electron and nuclear…
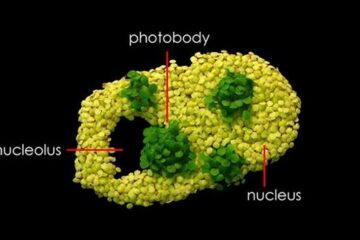
Free-forming organelles help plants adapt to climate change
Scientists uncover how plants “see” shades of light, temperature. Plants’ ability to sense light and temperature, and their ability to adapt to climate change, hinges on free-forming structures in their…





















