Rating your pain from 0 to 10 might not help your doctor

In a study that appears in the October issue of the Journal of General Internal Medicine, they evaluate the usefulness of a scale that asks patients in primary care to rate their current pain from 0 (no pain) to 10 (worst pain).
Universal pain screening is an increasingly common practice, largely because of the Joint Commission on Accreditation of Healthcare Organization’s requirement that accredited hospitals and clinics routinely assess all patients for pain. JCAHO is the nation’s predominant standards-setting and accrediting body in health care.
“Our study is the first to evaluate the accuracy of the widely-used numeric rating scale [NRS] as a screening test to identify primary care patients with clinically important pain. Accurate screening is important because pain symptoms, both serious and not so serious, are among the most common complaints in primary care,” said Erin E. Krebs, M.D., M.P.H., assistant professor of medicine at the IU School of Medicine and a Regenstrief Institute research scientist. “To be helpful, a screening test needs to provide accurate information that doctors can use to improve care. If a test isn’t very accurate or useful, doctors learn to tune out the numbers.”
The authors found that, while the NRS is easy to administer, it fails to identify about a third of patients with pain serious enough to impair day-to-day functioning. Most patients in this study had long-standing pain, and many had more than one pain problem. The authors did not evaluate the accuracy of pain ratings in settings where short-term pain is more common, such as after surgery. The researchers noted that because it focuses on current pain, the NRS may miss intermittent symptoms. They also reported that “pain” was not the preferred word for some patients. For example, one study participant indicated that he felt discomfort, but not pain.
“Universal pain screening has become widespread despite a lack of research evaluating its accuracy and effectiveness. We know that pain is a serious problem in primary care, but pain screening may not be the best way to address this problem,” said Dr. Krebs, who is also with the Center on Implementing Evidence-based Practice at the Roudebush Veterans Affairs Medical Center in Indianapolis.
The Robert Wood Johnson Foundation funded the study.
Media Contact
More Information:
http://www.iupui.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

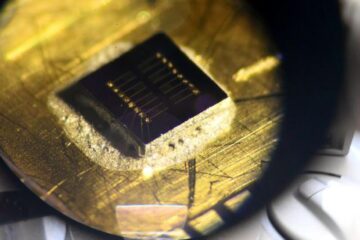
Sea slugs inspire highly stretchable biomedical sensor
USC Viterbi School of Engineering researcher Hangbo Zhao presents findings on highly stretchable and customizable microneedles for application in fields including neuroscience, tissue engineering, and wearable bioelectronics. The revolution in…

Twisting and binding matter waves with photons in a cavity
Precisely measuring the energy states of individual atoms has been a historical challenge for physicists due to atomic recoil. When an atom interacts with a photon, the atom “recoils” in…
Nanotubes, nanoparticles, and antibodies detect tiny amounts of fentanyl
New sensor is six orders of magnitude more sensitive than the next best thing. A research team at Pitt led by Alexander Star, a chemistry professor in the Kenneth P. Dietrich…





















