Ophthalmologists implant five patients with artificial silicon retina microchip

Solar Cell Implant May Restore Some Sight for the Blind
Ophthalmologists at Rush University Medical Center implanted Artificial Silicon Retina (ASR) microchips in the eyes of five patients to treat vision loss caused by retinitis pigmentosa (RP). The implant is a silicon microchip 2mm in diameter and one-thousandth of an inch thick, less than the thickness of a human hair. Four patients had surgery Tuesday, January 25. The fifth patient is scheduled for a later date.
Rush principal investigator Dr. John Pollack performed the surgeries with Dr. Kirk Packo, Dr. Pauline Merrill, Dr. Mathew MacCumber, and Dr. Jack Cohen. All are members of Illinois Retina Associates, S.C., a private practice group and are on the Rush faculty. Patients leave the hospital the same day and will be followed for two years as part of the study, and then indefinitely. The patients were recruited from a pool of about 5,000 applicants.
The implants are designed for people with retinal diseases such as macular degeneration and retinitis pigmentosa, which cause blindness and vision impairment in about 10 million Americans. More than one million of these people are legally blind.
“As is commonly seen in with retinitis pigmentosa, these patients all have severe narrowing of their visual fields down to a very small central circle, and all patients in the study are legally blind,” says Pollack.
The Artificial Silicon RetinaTM (ASR) was invented by Dr. Alan Chow, pediatric ophthalmologist and Rush faculty member, who developed the chip and founded Optobionics, with his brother Vincent, vice president of engineering. Optobionics is located in Naperville, Illinois.
“This is an expansion of the study of the first 10 patients completed in 2002,” says study investigator Dr. Kirk Packo, who oversees the three participating sites. The sites are Johns Hopkins School of Medicine, Baltimore, Emory University School of Medicine/Atlanta VA Medical Center and Rush.
Pollack says the current protocol has been modified to reduce the likelihood of inadvertant scientific bias. “We operated on the right eye of each of the initial 10 patients. For the next 20 patients we will randomly select which eye will receive the ASR chip. In addition, post-operative vision testers will be masked as to which eye received the ASR chip implant. The current study is being performed at these study centers in order to independently validate previous studies performed by Optobionics.”
The first 10 patients all reported some degree of improvement in visual function, says Pollack. “Improvement in visual function was variable and included the ability to read letters, improvement in color vision, and expansion of their visual field. Some patients gained new ability to recognize facial features — something that they were unable to do before ASR chip implantation. Some patients have experienced improvement in activities of daily living such as improved ambulation-not bumping into objects around the house, and reading the time on a clock.”
Still in Phase II clinical trials, Pollack cautions it is still too early to determine what percentage of patients might experience improvement in vision and what resolution capability these patients might eventually have. “Although we hope that all patients receiving the chip will experience some improvement in visual function, we can’t say for sure how these patients will respond to this new treatment since this is still an experimental trial. If this study and future studies show safety and efficacy of the chip and it’s approved by the FDA, it could be as soon as three to five years that this technology would be available to others.”
Surgical Information
The ASR chip contains approximately 5,000 microscopic solar cells that convert light into electrical impulses. The purpose of the chip is to replace damaged photoreceptors, the “light-sensing” cells of the eye, which normally convert light into electrical signals within the retina. Loss of photoreceptor cells occurs in persons with retinitis pigmentosa (RP) and other retinal diseases.
The microsurgical procedure starts with three tiny incisions in the white part of the subject’s eye, each incision no larger than the diameter of a needle. Through these incisions, the surgeons insert a miniature cutting and vacuuming device that removes the gel in the middle of the eye and replaces it with saline. They then make a pinpoint opening in the retina through which they inject fluid to lift up a portion of the retina from the back of the eye, creating a small pocket in the “subretinal space” just wide enough to accommodate the ASR.
The surgeons then enlarge the pocket opening and insert the implant into the subretinal space. Finally, they reseal the retina over the ASR, insert air into the middle of the eye to gently push the retina back down over the device, and close the incisions. Over a period of 1 week the air bubble is resorbed and replaced by fluids created within the eye.
According to Chow, “The use of the subretinal space to hold a device that artificially stimulates the retina seems a logical step in replacing the loss of photoreceptor cells of the retina. If the implant is tolerated well and is able to successfully stimulate the retina, it may open up new opportunities for restoring sight in patients with the end stages of retinitis pigmentosa.”
Media Contact
More Information:
http://www.rush.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
Microscopic basis of a new form of quantum magnetism
Not all magnets are the same. When we think of magnetism, we often think of magnets that stick to a refrigerator’s door. For these types of magnets, the electronic interactions…

An epigenome editing toolkit to dissect the mechanisms of gene regulation
A study from the Hackett group at EMBL Rome led to the development of a powerful epigenetic editing technology, which unlocks the ability to precisely program chromatin modifications. Understanding how…
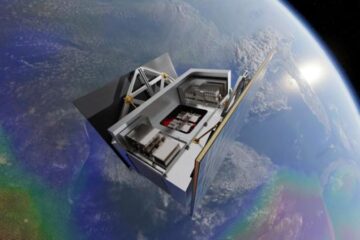
NASA selects UF mission to better track the Earth’s water and ice
NASA has selected a team of University of Florida aerospace engineers to pursue a groundbreaking $12 million mission aimed at improving the way we track changes in Earth’s structures, such…





















