Penn Medicine's 'sepsis sniffer' generates faster sepsis care and suggests reduced mortality

Craig A. Umscheid, M.D., M.S.C.E., is the director of Penn's Center for Evidence-based Practice. Credit: Penn Medicine
An automated early warning and response system for sepsis developed by Penn Medicine experts has resulted in a marked increase in sepsis identification and care, transfer to the ICU, and an indication of fewer deaths due to sepsis. A study assessing the tool is published online in the Journal of Hospital Medicine.
Sepsis is a potentially life-threatening complication of an infection; it can severely impair the body's organs, causing them to fail. There are as many as three million cases of severe sepsis and 750,000 resulting deaths in the United States annually. Early detection and treatment, typically with antibiotics and intravenous fluids, is critical for survival.
The Penn prediction tool, dubbed the “sepsis sniffer,” uses laboratory and vital-sign data (such as body temperature, heart rate, and blood pressure) in the electronic health record of hospital inpatients to identify those at risk for sepsis. When certain data thresholds are detected, the system automatically sends an electronic communication to physicians, nurses, and other members of a rapid response team who quickly perform a bedside evaluation and take action to stabilize or transfer the patient to the intensive care unit if warranted.
The study developed the prediction tool using 4,575 patients admitted to the University of Pennsylvania Health System (UPHS) in October 2011. The study then validated the tool during a pre-implementation period from June to September 2012, when data on admitted patients was evaluated and alerts triggered in a database, but no notifications were sent to providers on the ground. Outcomes in that control period were then compared to a post-implementation period from June to September 2013. The total number of patients included in the pre and post periods was 31,093.
In both the pre- and post-implementation periods, four percent of patient visits triggered the alert. Analysis revealed 90 percent of those patients received bedside evaluations by the care team within 30 minutes of the alert being issued. In addition, the researchers found that the tool resulted in:
- A two to three-fold increase in orders for tests that could help identify the presence of sepsis
- A 1.5 to two-fold increase in the administration of antibiotics and intravenous fluids
- An increase of more than 50 percent in the proportion of patients quickly transferred to the ICU
- A 50 percent increase in documentation of sepsis in the patients' electronic health record
The study found a lower death rate from sepsis and an increase in the number of patients successfully discharged home, although these findings did not reach statistical significance.
“Our study is the first we're aware of that was implemented throughout a multihospital health system,” said lead author Craig A. Umscheid, MD, MSCE, director of Penn's Center for Evidence-based Practice. “Previous studies that have examined the impact of sepsis prediction tools at other institutions have only taken place on a limited number of inpatient wards. The varied patient populations, clinical staffing, practice models, and practice cultures across our health system increases the generalizability of our findings to other health care settings.”
Umscheid also noted that the tool could help triage patients for suitability of ICU transfer. “By better identifying those with sepsis requiring advanced care, the tool can help screen out patients not needing the inevitably limited number of ICU beds.”
###
In addition to Umscheid, the other Penn co-authors are Joel Betesh, MD; Christine Vanzandbergen, PA, MPH; Asaf Hanish, MPH; Gordon Tait, BS; Mark E. Mikkelsen, MD, MSCE; Benjamin French, PhD; and Barry D. Fuchs, MD, MS.
Dr. Umscheid's contribution to this project was supported in part by the National Institutes of Health, National Center for Advancing Translational Sciences, grant # UL1TR000003.
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $4.3 billion enterprise.
The Perelman School of Medicine has been ranked among the top five medical schools in the United States for the past 17 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $392 million awarded in the 2013 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania — recognized as one of the nation's top “Honor Roll” hospitals by U.S. News & World Report; Penn Presbyterian Medical Center; Chester County Hospital; Penn Wissahickon Hospice; and Pennsylvania Hospital — the nation's first hospital, founded in 1751. Additional affiliated inpatient care facilities and services throughout the Philadelphia region include Chestnut Hill Hospital and Good Shepherd Penn Partners, a partnership between Good Shepherd Rehabilitation Network and Penn Medicine.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2013, Penn Medicine provided $814 million to benefit our community.
Media Contact
More Information:
http://www.uphs.upenn.edu/news/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
Why getting in touch with our ‘gerbil brain’ could help machines listen better
Macquarie University researchers have debunked a 75-year-old theory about how humans determine where sounds are coming from, and it could unlock the secret to creating a next generation of more…
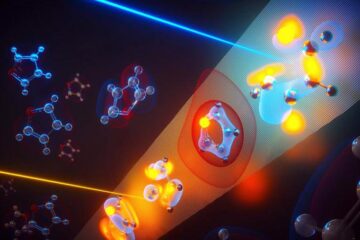
Attosecond core-level spectroscopy reveals real-time molecular dynamics
Chemical reactions are complex mechanisms. Many different dynamical processes are involved, affecting both the electrons and the nucleus of the present atoms. Very often the strongly coupled electron and nuclear…
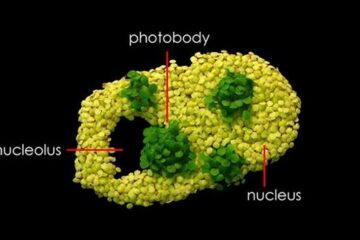
Free-forming organelles help plants adapt to climate change
Scientists uncover how plants “see” shades of light, temperature. Plants’ ability to sense light and temperature, and their ability to adapt to climate change, hinges on free-forming structures in their…





















