New Compound Prevents First Steps of Fungal Infection
Right, C. albicans in its ovoid, harmless state; left, the infectious, filamented state.<br>
Targeting serious and sometimes deadly fungal infections, a team of researchers at Worcester Polytechnic Institute (WPI) and the University of Massachusetts Medical School (UMMS) has discovered a chemical compound that prevents fungal cells from adhering to surfaces, which, typically, is the first step of the infection process used by the human pathogen Candida albicans (C. albicans).
After screening 30,000 chemical compounds in a series of tests with live C. albicans, the team found one molecule that prevented the yeast from adhering to human cells or to polystyrene, a common plastic used in many medical devices. Named “filastatin” by the researchers, this molecule now emerges as a candidate for new anti-fungal drug development and as a potential protective material to embed on the surfaces of medical devices to prevent fungal infections.
The team, led by co-principal investigators Paul Kaufman, PhD, professor of molecular medicine at UMMS, and Reeta Rao, PhD, associate professor of biology and biotechnology at WPI, reports its findings in the paper “Chemical screening identifies filastatin, a small molecule inhibitor of Candida albicans adhesion, morphogenesis, and pathogenesis,” published online in advance of print by the journal Proceedings of the National Academy of Sciences (PNAS).
“In humans, the most widespread fungal pathogen is Candida albicans, which is also one of the most frequent causes of hospital-acquired infections,” the authors write. “We conclude that filastatin is not toxic to the human cell line under our assay conditions, but is unique in that it can impair fungal adhesion both to inert surfaces and to cultured human epithelial cells.”
Infection by C. albicans causes common chronic illnesses like thrush and vaginitis, which affect millions of people globally each year and are not easily cleared by the handful of anti-fungal drugs now available. While most fungal infections do not cause serious harm, if one spreads to the bloodstream it can be deadly.
Hospitalized patients with catheters or central intravenous lines are at risk as the fungi can grow on those devices and enter the body. Similarly, patients with implanted medical devices like pacemakers or prosthetic hips or knees are also at risk if the implant carries a fungus into the body. Also, people with compromised immune systems are at greater risk for serious fungal infections. Because of the lack of effective drugs against C. albicans and other pathogenic fungi, the mortality rate for systemic fungal infections is between 30 and 50 percent.
Typically, a blood stream infection of C. albicans or a similar pathogen begins with fungal cells attaching to a surface—a catheter, for example, or epithelial cells lining the mouth—to form what is known as a biofilm. Next, the ovoid shaped yeast cells morph into an invasive filamentous form, extending pointed filaments that penetrate and damage surrounding tissues. In the current study, the team found that filastatin curtailed both steps: it largely prevented C. albicans from adhering to various surfaces, and it significantly reduced filamentation (inspiring the name filastatin).
As a next step, the team tested filastatin's impact on C. albicans cells that had grown unfettered in test wells and had already adhered to the polystyrene walls. When the compound was added to the culture mix, it knocked off many of the fungal cells already stuck to the polystyrene. The inhibitory effects of filastatin were further tested on human lung cells, mouse vaginal cells, and live worms (C. elgans) exposed to the fungus to see if it would reduce adhesion and infection. In all cases, the novel small molecule had significant protective effects without showing toxicity to the host tissues.
Research is now focused on teasing out the precise molecular mechanisms filastatin uses to prevent adhesion and filamentation. “We need to find the target of this molecule,” Rao said. “We have some good leads, and the fact that we aren’t seeing toxicity with host cells is very encouraging, but there is more work to be done.”
Additional studies on filastatin are underway at both WPI and UMMS. “The molecule affects multiple clinically relevant species, so we're pursuing the idea that it provides a powerful probe into what makes these organisms efficient pathogens,” Dr. Kaufman said. “In this era of budget gridlock in Washington, our ability to get funding from the Center for Clinical and Translational Research at UMMS to support this work was essential for allowing us to pursue our ideas for novel ways to approach this important class of hospital-acquired infections.”
The project was also funded by a grant from a WPI/UMMS pilot program established to promote collaborations between researchers at the universities to advance early stage translational research. “Joint research programs, such as the pilot program between our institutions, are central to WPI's work in the life sciences,” said Michael Manning, PhD, associate provost for research ad interim, at WPI. “As this collaboration between Professors Rao and Kaufman demonstrates so well, both institutions can leverage their complementary expertise for the ultimate advancement of scientific discovery and public health.”
Terence R. Flotte, MD, UMMS executive deputy chancellor, provost, and dean of the School of Medicine, agreed. “The faculty of UMass Medical School and WPI possess scientific knowledge and expertise in disciplines that complement each other,” he said. “The creation of this type of multidisciplinary team collaboration between the two universities allows us to work synergistically to solve problems important for improving human health.”
Media Contact
More Information:
http://www.wpi.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
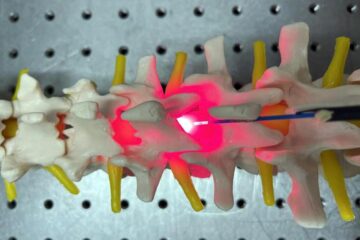
Red light therapy for repairing spinal cord injury passes milestone
Patients with spinal cord injury (SCI) could benefit from a future treatment to repair nerve connections using red and near-infrared light. The method, invented by scientists at the University of…
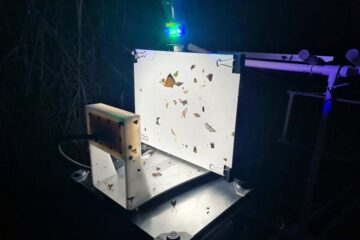
Insect research is revolutionized by technology
New technologies can revolutionise insect research and environmental monitoring. By using DNA, images, sounds and flight patterns analysed by AI, it’s possible to gain new insights into the world of…

X-ray satellite XMM-newton sees ‘space clover’ in a new light
Astronomers have discovered enormous circular radio features of unknown origin around some galaxies. Now, new observations of one dubbed the Cloverleaf suggest it was created by clashing groups of galaxies….





















