Gene Therapy "Trains" Immune System to Destroy Brain Cancer Cells

A new gene therapy approach that attracts and “trains” immune system cells to destroy deadly brain cancer cells also provides long-term immunity, produces no significant adverse effects and — in the process of destroying the tumor — promotes the return of normal brain function and behavioral skills, according to a study conducted by researchers at Cedars-Sinai Medical Center’s Board of Governors Gene Therapeutics Research Institute.
The study was conducted in a recently developed laboratory rat model of glioblastoma multiforme (GBM) that closely simulates outcomes in humans and supports the translation of this procedure to human clinical trials later this year. Results of the study are described in the Feb. 19 issue of Molecular Therapy, the journal of the American Society for Gene Therapy.
“These findings appear to be a significant milestone in creating an effective treatment for glioblastoma multiforme,” said Maria Castro, Ph.D., co-director of the Board of Governors Gene Therapeutic Research Institute and principal investigator of the study. “This therapy significantly improved survival rate, induced long-lasting systemic anti-tumor immunity, and resolved the neuropathological abnormalities caused by the tumors, which has been a stumbling block to many promising treatments.”
The article documents the gene therapy’s effectiveness in killing GBM cells and launching an effective and sustained systemic immune response. It also focuses on the safety of the therapy as well as its ability to restore normal brain function and reverse behavioral deficits caused by large tumors.
Humans with GBM often suffer behavioral abnormalities that affect concentration, memory and balance. In the animal studies, rats exhibited abnormal rotational movements. The research team found that as the tumors grew, they displaced and compressed nerve terminals and impulse-conducting axons. But long-term survivors who had received the gene therapy did not have long-term injury or behavioral impairment resulting from the tumor or the treatment.
“Tumor growth causes behavioral deficits, but even treatments, such as chemotherapy and radiation therapy, can cause learning disabilities and other cognitive problems. In our animal study, this therapy eliminated the tumor mass and reversed the deficits that were caused by the tumor,” said Pedro Lowenstein, M.D., Ph.D., co-principal investigator on the study and director of the Board of Governors Gene Therapeutics Research Institute.
Glioblastoma multiforme, the most common and deadly type of brain cancer, usually claims the lives of victims within six to 12 months of diagnosis. It is extremely difficult to treat for a variety of reasons. GBM tumors grow rapidly, often becoming large before a diagnosis is made. Also, cells readily infiltrate neighboring tissue and migrate to other areas, hampering complete surgical removal. Chemotherapy and radiation therapy are unable to eliminate all residual GBM cells, which frequently become resistant to the treatments.
The blood-brain barrier also prevents chemotherapy from effectively reaching tumor cells, and key cells needed to launch and sustain a systemic anti-tumor immune response – dendritic cells, or antigen-presenting cells – do not naturally occur within the brain.
The gene therapy approach developed at Cedars-Sinai sidesteps all of these challenges. The researchers used a virus stripped of its disease-causing genes as a vehicle to deliver two therapeutic proteins directly into the tumor cells. One protein, FMS like tyrosine kinase 3 ligand (Flt3L), drew dendritic cells into the brain. Another protein, herpes simplex virus type 1 thimidine kinase (HSV1-TK), combined with the antiviral gancyclovir (GCV), killed tumor cells.
Dendritic cells clean up debris from dying cells and in the process alert immune system cells of the existence of foreign entities, or antigens – in this case, GBM cells. Newly “educated” immune system cells then swarm to the tumor cells to destroy them.
In an earlier study, the Cedars-Sinai researchers used HSV1-TK and GCV alone to treat GBM and found that about 20 percent of the animals survived, compared to controls. By adding the dendritic-cell inducing Flt3L, the survival rate jumped to about 70 percent. Systemic immune activity was sustained, even fending off a “re-challenge” with additional tumor cells. In this study, the researchers at the BOG-GTRI reported that this therapy could also revert behavioral abnormalities caused by the growing tumor in the brain.
“In the fairly near future, this combined gene therapy may work synergistically with current therapies, including chemotherapy and radiation therapy, allowing doctors to reduce dosages and avoid side effects,” Dr. Castro said. “But with the safety, effectiveness and curative potential seen in these studies, we are hopeful that gene therapy for GBM could become the new standard of care.”
The study was supported by National Institutes of Health/National Institute of Neurological Disorders and Stroke, The Bram and Elaine Goldsmith and the Medallions Group Endowed Chairs in Gene Therapeutics, the Linda Tallen & David Paul Kane Foundation Annual Fellowship, and the Board of Governors at Cedars-Sinai.
Citation: Cancer Research, Combined immune-stimulation and conditional cytoxic gene therapy provide long term survival in a large glioma model (August 2005).
Media Contact
More Information:
http://www.cedars-sinai.eduAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
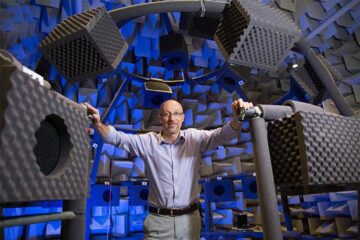
Why getting in touch with our ‘gerbil brain’ could help machines listen better
Macquarie University researchers have debunked a 75-year-old theory about how humans determine where sounds are coming from, and it could unlock the secret to creating a next generation of more…
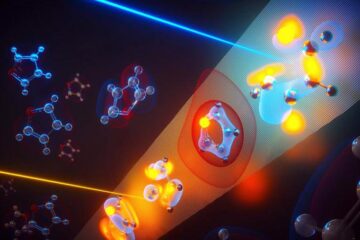
Attosecond core-level spectroscopy reveals real-time molecular dynamics
Chemical reactions are complex mechanisms. Many different dynamical processes are involved, affecting both the electrons and the nucleus of the present atoms. Very often the strongly coupled electron and nuclear…
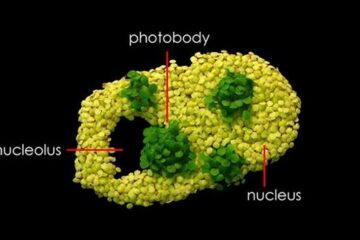
Free-forming organelles help plants adapt to climate change
Scientists uncover how plants “see” shades of light, temperature. Plants’ ability to sense light and temperature, and their ability to adapt to climate change, hinges on free-forming structures in their…





















