
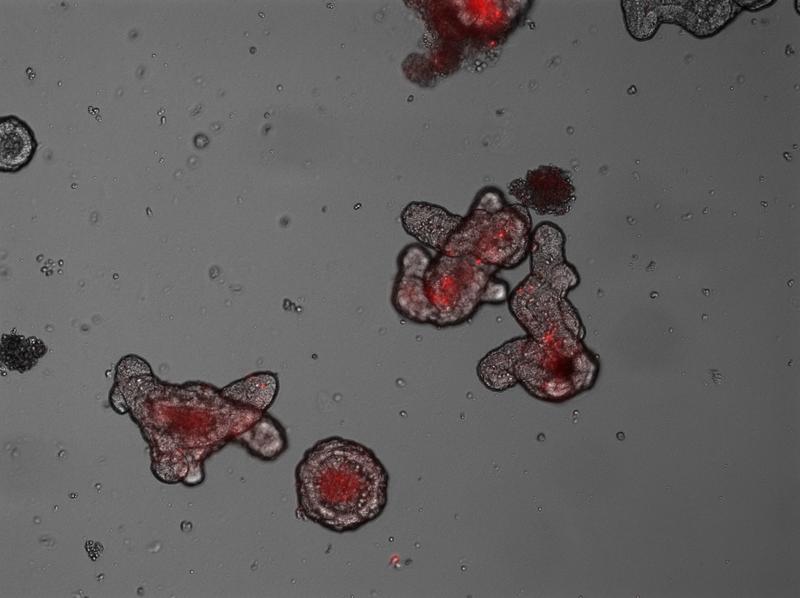
Organoids, here with 400x magnification under a microscope, function partially like real bowels. The mini-bowel for research is made from stem cells in the laboratory.
Photo: Konrad Aden/IKMB
20 percent of all patients with Crohn's disease, a clinical subtype of inflammatory bowel disease, have a mutation in the gene ATG16L1. This gene is involved in a cellular process called autophagy, which functions as a recycling mechanisms of aged organelles and macromolecules within cells.
The delineation of the molecular consequences of Atg16l1 mutations on host immune system has been investigated in the Cluster of Excellence “Inflammation at Interfaces” for a long time.
Now, a team led by Cluster Board Member Professor Philip Rosenstiel and Dr Konrad Aden from the Institute of Clinical Molecular Biology (IKMB) at Kiel University and the Department of Internal Medicine I, UKSH Kiel have made a discovery with on a novel function of Atg16l1, which sheds a new light on the pathogenesis of IBD and might help to refine future treatment of IBD patients.
Starting point for the study, which has been published in the Journal of Experimental Medicine, is a new therapeutic approach for people with chronic inflammatory bowel diseases. The biological compound Interleukin 22 is an immune cell derived cytokine and has been well known for its regenerative effect on the intestinal mucosa. Now, the therapeutic potential of this cytokine is currently tested in clinical studies in IBD patients .
“Interleukin 22 is one of the key barrier protective cytokines which promotes regeneration of the intestinal mucosa. There was evidence that the intestinal mucosa is protected from certain stress reactions by IL-22. The principle is in the first stages of clinical testing,” said Cluster spokesperson Professor Stefan Schreiber, Director of the Department of Internal Medicine I at the UKSH Kiel.
The risk gene for Crohn's disease, ATG16L1 is involved in this particular type of cell stress. The loss of function of the gene leads to reduced degradation of aged proteins, and thus to increased inflammation. ” In light of this background we wanted to know whether proper Atg16l1 function is essential for mediating regenerative IL-22 responses in the intestinal epithelium ?” said Schreiber.
The authors investigated this central question mice carrying a knock out of the Atg16l1 gene specifically in intestinal epithelial cells. According to the lead author Dr Konrad Aden, they came to a very surprising result: “Essentially, Interleukin 22 stimulates cell growth and promotes regeneration of the intestinal mucosa. However, intestinal epithelial cells that carry a deletion of ATG16L1 in the intestinal epithelium, behave in the exact opposite way. In this case, Interleukin 22 causes a stress response in the cells, and a paradoxical cell death.”
Thus, in the presence of the gene mutation, the desired protective function of Interleukin 22 is transformed into a pro-inflammatory effect. Although the study did not explicitly examine whether the known Atg16l1 variants also lead to paradoxical interleukin 22 effects in humans, it is tempting to speculate that there is relevance also for patients.
“This finding can help us to understand the complex changes in the intestinal barrier organ, which occur in chronic intestinal inflammation. In addition to pure regeneration, IL-22 is also involved in cellular programmes, which control the body's own antibiotics, and thus the intestinal flora – a delicate interaction that is disturbed in IBD. We now need to carefully examine this in humans, since it may enable a new approach for more targeted treatment,” said Professor Philip Rosenstiel.
Many of the tests were performed on so-called intestinal organoids. These mini-guts are three-dimensional structures created from intestinal stem cells, embedded in a solid matrix and supplemented with special growth factors. They can be obtained from intestinal biopsies in mice and humans, and kept for a long time in the laboratory.
“These organoids are much closer to the physiology of the respective disease than a cell culture. In addition, they are something very individual. We expect that this in vitro technology will also be used in future to test the individual effectiveness of treatments in advance, and thereby avoid unnecessary treatments for patients,” Aden said.
Original publication
Konrad Aden et al. ATG16L1 orchestrates interleukin-22 signaling in the intestinal epithelium via 2 cGAS/STING. Journal of Experimental Medicine. Published September 25, 2018. http://jem.rupress.org/content/early/2018/09/26/jem.20171029
Contact:
Dr Konrad Aden
The Department of Internal Medicine I, UKSH Kiel
Institute of Clinical Molecular Biology, Kiel University
Tel.: 0431/500- 15167
k.aden@ikmb.uni-kiel.de
Prof. Dr Philip Rosenstiel
Institute of Clinical Molecular Biology, Kiel University
Tel.: +49 (0)431 500 15111
p.rosenstiel@mucosa.de
Photos are available to download:
http://inflammation-at-interfaces.de/de/newsroom/aktuelles/Aden.jpg
Konrad Aden
Konrad Aden, Cluster of Excellence “Inflammation at Interfaces”, specialist in internal medicine at the Department of Internal Medicine I at UKSH Kiel, and research associate at the Institute of Clinical Molecular Biology (IKMB), Faculty of Medicine at Kiel University. Photo: private
http://inflammation-at-interfaces.de/de/newsroom/aktuelles/copy_of_Rosenstiel.jp…
Philip Rosenstiel
Philip Rosenstiel, Cluster of Excellence “Inflammation at Interfaces”, Professor of Molecular Medicine at Kiel University and Director of the Institute of Clinical Molecular Biology (IKMB), Faculty of Medicine at Kiel University and the University Medical Center Schleswig-Holstein (UKSH), Campus Kiel. Photo: Tebke Böschen / Cluster of Excellence “Inflammation at Interfaces”
http://inflammation-at-interfaces.de/de/newsroom/aktuelles/Organoide.png
Organoids
Organoids, here with 400x magnification under a microscope, function partially like real bowels. The mini-bowel for research is made from stem cells in the laboratory, which were previously removed from the bowel tissue of humans or lab animals by means of colonoscopy. Photo: Konrad Aden/IKMB
Press contact:
Kerstin Nees
Tel.: (040) 8320998, E-mail: presse.cluster@uv.uni-kiel.de
Website: www.inflammation-at-interfaces.de
The Cluster of Excellence “Inflammation at Interfaces” has been funded since 2007 by the Excellence Initiative of the German Government and the federal states with a total budget of 68 million Euros. It is currently in its second phase of funding. Around 300 cluster members are spread across the four locations: Kiel (Kiel University, University Medical Center Schleswig-Holstein (UKSH), Muthesius University of Fine Arts and Design (MHK)), Lübeck (University of Lübeck, UKSH), Plön (Max Planck Institute for Evolutionary Biology) and Borstel (Research Center Borstel (FZB) – Center for Medicine and Biosciences) and are researching an innovative, systematic approach to the phenomenon of inflammation, which can affect all barrier organs such as the intestines, lungs and skin.
Cluster of Excellence “Inflammation at Interfaces”
Scientific Office, Head: Dr habil. Susanne Holstein
Postal address: Christian-Albrechts-Platz 4, 24118 Kiel, Germany
Contact: Sonja Petermann
Tel.: +49 (0)431 880-4850, Fax: +49 (0)431 880-4894
E-mail: spetermann@uv.uni-kiel.de
Twitter: I@I @medinflame
http://inflammation-at-interfaces.de/en/newsroom/current-issues/faulty-digestion…
Dr Konrad Aden
The Department of Internal Medicine I, UKSH Kiel
Institute of Clinical Molecular Biology, Kiel University
Tel.: 0431/500- 15167
k.aden@ikmb.uni-kiel.de
Prof. Dr Philip Rosenstiel
Institute of Clinical Molecular Biology, Kiel University
Tel.: +49 (0)431 500 15111
p.rosenstiel@mucosa.de












