Cells passed from mother to child during pregnancy live on and make insulin

The phenomenon is known as microchimerism, and it is still unclear as to whether the presence of such cells can be harmful to the recipient. A Bristol team has looked for maternal cells in children with type 1 diabetes, an immune-mediated disorder, and found that around 20 per cent of these children have unusually high levels of maternal DNA in their circulation. An even more surprising finding is that some maternal cells have entered the child's pancreas and are functioning there as insulin-producing beta cells. The study, initially undertaken in the belief that maternal cells might trigger autoimmunity in the child, has now taken an interesting new twist, for the maternal cells might even be helping the child to repair injury.
In this study, published in the January 22 issue of the Proceedings of the National Academy of Sciences, Dr Kathleen Gillespie and Professor Edwin Gale from the Department of Clinicl Science @ North Bristol in collaboration with Professor J. Lee Nelson and colleagues at Fred Hutchinson Cancer Research Center, Seattle, found no evidence that the mother's cells were attacking the child's insulin cells and no evidence that the maternal cells were targets of an immune response from the child's immune system.
Instead, the researchers found a small number of female islet beta cells in male pancreatic tissue (procured from autopsies) that produced insulin. Microchimerism is the term used when an individual harbors cells or DNA that originate from another genetically distinct individual. “To our knowledge a maternal contribution to endocrine function has not previously been described,” the authors said. “Our findings also raise the possibility that naturally acquired microchimerism might be exploited to therapeutic benefit.”
The study also found significantly higher levels of maternal DNA in the peripheral blood of 94 children and adults with Type 1 diabetes as compared to 54 unaffected siblings and 24 unrelated healthy subjects they studied.
Originally, the study of 172 individuals and pancreatic tissue from four males was designed to ask the question whether small numbers of maternal cells might be involved in any way in Type 1 diabetes. “Our initial theory was that perhaps, in some situations, too many cells cross from mother to fetus in pregnancy. Could diabetes result because the child lost tolerance to those cells because they are genetically half foreign? Our research appears to disprove this,” said Professor Gale. “It is possible that the maternal cells may even be helping to regenerate damaged tissue in the pancreas.”
The investigators are excited about the observation that maternal microchimerism results in cells that make insulin – these maternal stem cells could provide new insights into how insulin producing beta cells are generated.
Media Contact
More Information:
http://www.bristol.ac.ukAll latest news from the category: Studies and Analyses
innovations-report maintains a wealth of in-depth studies and analyses from a variety of subject areas including business and finance, medicine and pharmacology, ecology and the environment, energy, communications and media, transportation, work, family and leisure.
Newest articles
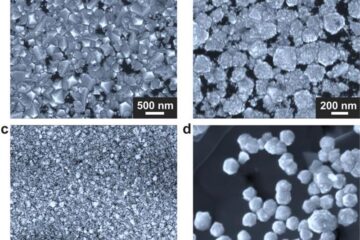
Making diamonds at ambient pressure
Scientists develop novel liquid metal alloy system to synthesize diamond under moderate conditions. Did you know that 99% of synthetic diamonds are currently produced using high-pressure and high-temperature (HPHT) methods?[2]…
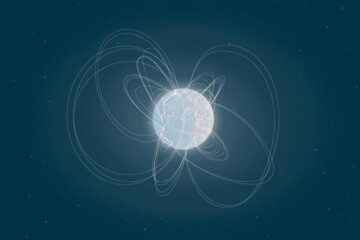
Eruption of mega-magnetic star lights up nearby galaxy
Thanks to ESA satellites, an international team including UNIGE researchers has detected a giant eruption coming from a magnetar, an extremely magnetic neutron star. While ESA’s satellite INTEGRAL was observing…
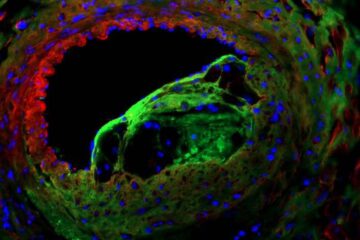
Solving the riddle of the sphingolipids in coronary artery disease
Weill Cornell Medicine investigators have uncovered a way to unleash in blood vessels the protective effects of a type of fat-related molecule known as a sphingolipid, suggesting a promising new…





















