Targeting tuberculosis 'hotspots' could have widespread benefit

An analysis of data from Rio de Janeiro showed that a reduction in TB infections within three high-transmission hotspots could reduce citywide transmission by 9.8 percent over 5 years, and as much as 29 percent over 50 years. The study was published May 28 by the journal PNAS.
“Targeting treatment of 'core groups' as a way to reduce community-wide transmission is common with diseases like HIV and malaria, but is less accepted as a mantra for TB control,” said David Dowdy, MD, PhD, ScM, lead author of the study and assistant professor in the Bloomberg School's Department of Epidemiology.
“Our findings suggest that hotspots containing 6 percent of a city's population can be responsible for 35 percent or more of its ongoing TB transmission. Controlling TB in these hotspots may have a similar impact on long-term, community-wide TB incidence as achieving the same targets in the remaining 94 percent of the population.”
For the study, Dowdy and his colleagues developed mathematical models for TB transmission using surveillance data from Rio de Janeiro. Each model tested different scenarios for TB transmission between the hotspot and the rest of the community. Co-infection with HIV was also factored into the model.
According to the study, reducing TB transmission rates in the hotspot to those in the general community reduced citywide TB incidence by a mean 2 percent per year over the first 5 years. By year 50, TB incidence was reduced by 29.7 percent, reflecting a 62.8 percent reduction in incidence in the hotspot and a 23.1 percent reduction in the remaining community.
Tuberculosis infects more than 8.8 million people worldwide, resulting in 1.4 million deaths each year. The disease is known to cluster in hotspots typically characterized by crowding, poverty and other illnesses such as HIV. Nevertheless, TB transmission appears to be more homogeneous than that of many other infectious diseases, in which 20 percent of the population may generate 80 percent of infections.
According to Dowdy, “TB may not follow the same '80/20' rule that we see in parasitic or sexually transmitted diseases, but the '35/6' rule seen in our study suggests that targeting hotspots is still the best way to control TB in a community.”
The authors of “Heterogeneity in tuberculosis transmission and the role of geographic hotspots in propagating epidemics” are David W. Dowdy, Jonathan E. Golub, Richard Chaisson and Valeria Saraceni.
The research was supported by the Bill & Melinda Gates Foundation.
Follow the Johns Hopkins Bloomberg School of Public Health on Facebook at www.facebook.com/JohnHopkinsSPH or on Twitter at www.twitter.com/JohnsHopkinsSPH.
Media Contact
More Information:
http://www.jhsph.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Properties of new materials for microchips
… can now be measured well. Reseachers of Delft University of Technology demonstrated measuring performance properties of ultrathin silicon membranes. Making ever smaller and more powerful chips requires new ultrathin…

Floating solar’s potential
… to support sustainable development by addressing climate, water, and energy goals holistically. A new study published this week in Nature Energy raises the potential for floating solar photovoltaics (FPV)…
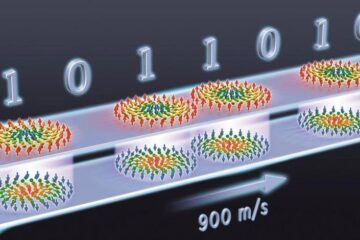
Skyrmions move at record speeds
… a step towards the computing of the future. An international research team led by scientists from the CNRS1 has discovered that the magnetic nanobubbles2 known as skyrmions can be…





















