Study suggests blood test for Alzheimer’s possible

Researchers from the University of Georgia, the Charlie Norwood VA Medical Center in Augusta and the Medical College of Georgia compared antibody levels in blood samples from 118 older adults with the participant’s level of dementia.
The team, whose results appear in the current edition of Journal of Gerontology: Medical Sciences, found that the concentration of two specific proteins that are involved in the immune response increases as the severity of dementia increases.
“We found a strong and consistent relationship between two particular antibodies and the level of impairment,” said study co-author L. Stephen Miller, professor and director of clinical psychology training in the UGA Franklin College of Arts and Sciences. “The finding brings us closer to our ultimate goal of developing a blood test that can diagnose Alzheimer’s disease or potentially identify if someone is at higher risk for the disease.”
Miller’s co-authors include Jennifer S. Wilson, a former undergraduate student in the UGA Honors program who is now pursing graduate studies at Emory University; Shyamala Mruthinti, research pharmacologist at the VA Medical Center and adjunct professor at MCG; and Jerry Buccafusco, director of the MCG Alzheimer’s Research Center. The team focused on antibodies that the body creates in response to two proteins that are associated with Alzheimer’s disease. One protein, known as amyloid-beta, forms the plaques that are evident in the brains of people with Alzheimer’s upon autopsy. The other protein, known as RAGE, is involved in the normal aging process but is expressed at higher levels in the brains of people with Alzheimer’s.
In a previous study that compared a group of people with Alzheimer’s disease to a healthy control group, Mruthinti and her colleagues found that anti-amyloid beta and anti-RAGE antibodies are significantly higher in the group with Alzheimer’s. The team’s latest study expands on that finding to reveal a direct relationship between severity of Alzheimer’s disease and levels of the two antibodies in the blood.
“Alzheimer’s is an inflammatory disease of the brain, and these two antibodies give us a way to measure that inflammation,” Mruthinti said. “Using them as an early diagnostic marker may allow us to start drug treatment early, when it’s most effective, to increase the patient’s quality of life.”
While optimistic about their findings, the researchers caution that it could still be years before a diagnostic test based on their work is clinically available. The study found that the relationship between the two antibodies and Alzheimer’s severity persists even after controlling for patient age and total antibody levels. To further test the strength of the relationship, the researchers are now working with a sample that controls for other factors that have the potential to influence levels of the two antibodies, such as diabetes and heart disease. Buccafusco and his colleagues are also working to decrease the cost and time involved in the test.
“We’re in the process of trying to reduce the test to a one-day procedure, whereas right now it takes three to four days,” Buccafusco said. “But even now, our test is orders of magnitude cheaper than having people come in every few months to get a functional MRI or PET scan to try to discern brain plaques.”
The team is targeting the two proteins themselves as a possible treatment for Alzheimer’s disease. Mruthinti explains that, individually, amyloid-beta and RAGE proteins don’t provoke an immune response. The trouble begins when the two bind and the immune system attacks, resulting in constant state of inflammation that damages the brain. The researchers recently developed a way to measure levels of amyloid beta-RAGE complex, and preliminary data using transgenic mice that express Alzheimer’s symptoms suggest that an antigen they created to boost the body’s natural immune response to the complex can reduce the formation of the brain plaques.
“The amyloid beta-RAGE complex cuts off the connections between neurons,” Mruthinti explained, “but our hope is that we can protect those connections by preventing those plaques from forming.”
The research was funded by a Merit Review Award from the Veterans Administration to principal investigator Mruthinti and by the Medical College of Georgia Alzheimer’s Research Center.
Media Contact
More Information:
http://www.uga.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Combatting disruptive ‘noise’ in quantum communication
In a significant milestone for quantum communication technology, an experiment has demonstrated how networks can be leveraged to combat disruptive ‘noise’ in quantum communications. The international effort led by researchers…
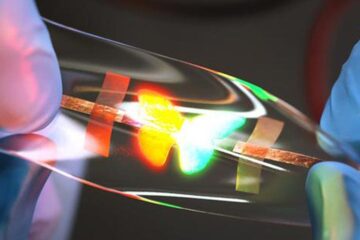
Stretchable quantum dot display
Intrinsically stretchable quantum dot-based light-emitting diodes achieved record-breaking performance. A team of South Korean scientists led by Professor KIM Dae-Hyeong of the Center for Nanoparticle Research within the Institute for…

Internet can achieve quantum speed with light saved as sound
Researchers at the University of Copenhagen’s Niels Bohr Institute have developed a new way to create quantum memory: A small drum can store data sent with light in its sonic…





















