Sick from your stomach: Bacterial changes may trigger diseases like rheumatoid arthritis

Larger-than-normal populations of specific gut bacteria may trigger the development of diseases like rheumatoid arthritis and possibly fuel disease progression in people genetically predisposed to this crippling and confounding condition, say the researchers, who are participating in the Mayo Illinois Alliance for Technology Based Healthcare.
The study is published in the April 2012 issue of PloS ONE.
“A lot of people suspected that gut flora played a role in rheumatoid arthritis, but no one had been able to prove it because they couldn't say which came first — the bacteria or the genes,” says senior author Veena Taneja, Ph.D., a Mayo Clinic immunologist. “Using genomic sequencing technologies, we have been able to show the gut microbiome may be used as a biomarker for predisposition.”
The roughly 10 trillion cells that make up the human body have neighbors: mostly bacteria that often help, training the immune system and aiding in digestion, for example. The bacteria in the intestines, in addition to a relatively small number of other microorganisms (the gut microbiome), outnumber human cells 10-to-1.
Researchers found that hormones and changes related to aging may further modulate the gut immune system and exacerbate inflammatory conditions in genetically susceptible individuals.
Nearly 1 percent of the world's population has rheumatoid arthritis, a disease in which the immune system attacks tissues, inflaming joints and sometimes leading to deadly complications such as heart disease. Other diseases with suspected gut bacterial ties include type I diabetes and multiple sclerosis.
Researchers with the Mayo Illinois Alliance for Technology Based Healthcare say that identifying new biomarkers in intestinal microbial populations and maintaining a balance in gut bacteria could help physicians stop rheumatoid arthritis before it starts.
“This study is an important advance in our understanding of the immune system disturbances associated with rheumatoid arthritis. While we do not yet know what the causes of this disease are, this study provides important insights into the immune system and its relationship to bacteria of the gut, and how these factors may affect people with genetic susceptibilities to disease,” says Eric Matteson, M.D., chairman of rheumatology at Mayo Clinic, who was not a study author.
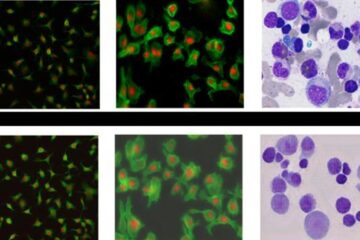
Dr. Taneja and her team genetically engineered mice with the human gene HLA-DRB1*0401, a strong indicator of predisposition to rheumatoid arthritis. A set of control mice were engineered with a different variant of the DRB1 gene, known to promote resistance to rheumatoid arthritis. Researchers used these mice to compare their immune responses to different bacteria and the effect on rheumatoid arthritis.
“The gut is the largest immune organ in the body,” says co-author Bryan White, Ph.D., director of the University of Illinois' Microbiome Program in the Division of Biomedical Sciences and a member of the Institute for Genomic Biology. “Because it's presented with multiple insults daily through the introduction of new bacteria, food sources and foreign antigens, the gut is continually teasing out what's good and bad.”
The gut has several ways to do this, including the mucosal barrier that prevents organisms — even commensal or “good” bacteria — from crossing the lumen of the gut into the human body. However, when commensal bacteria breach this barrier, they can trigger autoimmune responses. The body recognizes them as out of place, and in some way this triggers the body to attack itself, he says.
These mice mimic human gender trends in rheumatoid arthritis, in that females were about three times as likely to generate autoimmune responses and contract the disease. Researchers believe these “humanized” mice could shed light on why women and other demographic groups are more vulnerable to autoimmune disorders and help guide development of new future therapies.
“The next step for us is to show if bugs in the gut can be manipulated to change the course of disease,” Dr. Taneja says.
The study was funded by the Mayo-Illinois Alliance for Technology Based Healthcare and a grant from the U.S. Department of Defense.
Co-authors include Andres Gomez; Carl Yeoman, Ph.D.; and Margret Berg Miller, Ph.D., all of University of Illinois; David Luckey; Eric Marietta, Ph.D.; and Joseph Murray, M.D., all of Mayo Clinic.
About Mayo Clinic
Mayo Clinic is a nonprofit worldwide leader in medical care, research and education for people from all walks of life. For more information, visit www.mayoclinic.com and www.mayoclinic.org/news.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















