New targeted treatment for brain tumors shows promise in pre-clinical models

Monoclonal antibody targets key tumor growth factor; Successfully causes brain tumor regression and improves animal survival
Gliomas are the most common primary brain tumors, and also one of the most complicated cancers to treat. Currently, treatment options such as surgery, radiation and chemotherapy are only marginally beneficial and present significant risks for patients, including loss of physical and cognitive abilities. But, a new study published today in Clinical Cancer Research found that treatment with a novel monoclonal antibody (mAb) L2G7 inhibited the growth of glioma cells, induced glioma regression within the brain and prolonged survival – a finding that could be translated into human trials as early as next year.
“There is a tremendous need for advancement in the treatment of malignant brain tumors, which are the number one cancer killer of children under age 20 and a devastating diagnosis for adults as well,” said Dr. John Laterra, M.D., Ph.D., research scientist at the Kennedy Krieger Institute and senior author of the study. “The results of this study bring us closer to developing an alternative treatment option for both adults and for pediatric patients, who are hardest hit by conventional therapies.”
A team of researchers, led by Dr. Jin Kim of Galaxy Biotech, LLC in Mountain View, CA and Dr. John Laterra of the Kennedy Krieger Institute in Baltimore, MD, designed the study to evaluate the effectiveness of L2G7 in treating human gliomas implanted in mouse models. Results indicate that treatment with L2G7 completely inhibited the growth of the tumors when established under the skin of animals, while control mAb had only a minimal effect. Even more promising results were observed in mice with tumors implanted within the brain. In this setting, L2G7 not only induced tumor regression, but dramatically increased survival. Animals treated with the control all died within 41 days of starting the experiment. All mice treated with L2G7 survived through day 70, and 80% of the animals were alive at day 90, six weeks after stopping the L2G7 treatment.
L2G7 was developed by Dr. Kim’s team to inhibit the activities of hepatocyte growth factor (HGF). HGF is known to be a promising target for cancer therapy by virtue of its multiple actions that promote cancer malignancy. HGF stimulates tumor cell division, tumor angiogenesis (blood vessel formation) and tumor cell resistance to toxic agents such as chemotherapy and radiation. In this study, brain tumor cells were injected both under the skin and within the brain to specifically evaluate anti-tumor responses within the central nervous system. The central nervous system is a location often protected from cancer therapies by the “blood-brain barrier,” which could possibly limit the effects of mAb therapy on tumors situated within the brain. Treatment with L2G7 or a control mAb was given to both subsets of mice twice weekly.
In one experiment, the researchers delayed treatment of a subset of mice for 18 days to determine the effect of L2G7 on larger, more advanced tumors within the brain. At that time, the average tumor size was 26.7 mm3, but following only three doses of L2G7, tumors shrank to 11.7 mm3. Conversely, tumors treated with the control mAb grew 5-fold to 134.3 mm3 during the same period, with a mean volume 12 times larger than the L2G7-treated tumors.
“Monoclonal antibodies to growth factors or their receptors are playing an increasingly important role in cancer therapy,” said Dr. Cary Queen, President of Galaxy Biotech. “Because of its specificity for HGF, L2G7 may prove to be particularly effective at halting tumor growth while minimizing side effects and harm to the surrounding healthy brain cells.”
“Our company is committed to the clinical development of L2G7, and we hope to extend the current success of targeted antibody therapies in the treatment of breast, colon and lung cancer patients to the treatment of serious central nervous system malignancies such as gliomas.”
In a related study (Lal et al., Clin Cancer Res. 11:4479-4486, 2005), Dr. Laterra’s research team showed that targeting brain tumor HGF with gene therapy can substantially enhance the anti-tumor effects of radiation therapy, again emphasizing the important role HGF plays in brain tumors.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
Silicon Carbide Innovation Alliance to drive industrial-scale semiconductor work
Known for its ability to withstand extreme environments and high voltages, silicon carbide (SiC) is a semiconducting material made up of silicon and carbon atoms arranged into crystals that is…
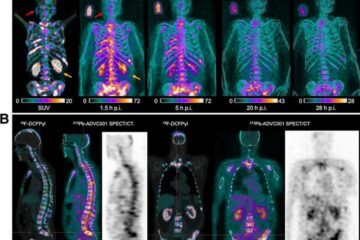
New SPECT/CT technique shows impressive biomarker identification
…offers increased access for prostate cancer patients. A novel SPECT/CT acquisition method can accurately detect radiopharmaceutical biodistribution in a convenient manner for prostate cancer patients, opening the door for more…

How 3D printers can give robots a soft touch
Soft skin coverings and touch sensors have emerged as a promising feature for robots that are both safer and more intuitive for human interaction, but they are expensive and difficult…





















