Autoimmune overload may damage HIV-infected brain

White blood cells may be cause of dementia in people with AIDS
Researchers studying the evolution of the human immunodeficiency virus (HIV) in the brain have found that the body’s own defenses may cause HIV-related dementia.
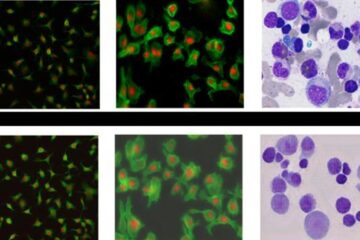
Publishing in the Sept. 2005 issue of the Journal of Virology, the researchers show that HIV in the temporal lobe mutates at a rate 100 times faster than in other parts of the body, triggering white blood cells to continually swarm to attack the infection. The associated overcrowding and inflammation appear to cause the dementia.
Earlier studies had suggested that the build-up of white blood cells could lead to HIV-related dementia, but this is the first study to track the probable mechanism.
The findings could lead to new treatments that target HIV-infected white blood cells, perhaps one day countering the brain wasting that will affect as many as 15 percent of the nearly 40 million people around the world who are infected with the virus.
The study is a collaboration among researchers at the University of California at Irvine, the University of Florida at Gainesville, Gene Johnson, Inc., of St. Augustine, Fla., the University of California at San Francisco (UCSF) and the University of Oxford in the United Kingdom.
One of the critical tools behind the discovery is HIVBase, a genetic data-storage and -analysis tool with which the researchers tracked the rapidly evolving viruses. Gene Johnson developed the tool with the support of an NSF Small Business Innovation Research award.
According to co-author Susanna Lamers of Gene Johnson and UCSF, the results strengthen an earlier hypothesis by Kenneth Williams of Harvard University and William Hickey of Dartmouth Medical School. They had suggested that the continual build-up of white blood cells in the brain could lead to HIV-associated dementia.
“In our work,” says Lamers, “we conducted a thorough examination of HIV genetic sequences and were able to prove that the researchers’ concept was a good explanation for both clinical latency–when the body mounts a strong immune defense and the number of viral particles decreases–and the long-term damage associated with HIV infection in the brain. They offered the model, we provided strong evidence that the model is accurate.”
Media Contact
More Information:
http://www.nsf.govAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















