Data show cyclosporine inhalation solution improves long-term survival in lung-transplant patients

Inhaled therapy addresses most common cause of death among lung-transplant recipients
Data presented for the first time today at the 25th Annual Meeting and Scientific Session of the International Society for Heart and Lung Transplantation (ISHLT) show that cyclosporine inhalation solution (CyIS) significantly improves long-term survival in lung-transplant patients compared to placebo. The data, which include 10-month follow-up statistics on patients originally enrolled in the pivotal study of CyIS, show that, with a median total follow-up of 53.3 months, CyIS-treated patients demonstrated a continued survival advantage over placebo-treated patients. Treatment with CyIS was associated with a 69 percent decrease in risk of death compared to placebo.
“Analysis of the pivotal study presented at ISHLT last year indicated that CyIS prevents chronic rejection, the most common cause of death in lung-transplant recipients. These follow-up data indicate that the significant survival advantage of CyIS compared to placebo persists long-term,” said Aldo Iacono, M.D., lead investigator of the study and Medical Director of the Lung Transplantation Program at University of Maryland Medical Center, Associate Professor of Medicine at the University of Maryland School of Medicine. “Despite the medical community’s best efforts, currently available immunosuppressive regimens have not been effective in reducing the incidence of chronic rejection or prolonging survival in lung-transplant patients. CyIS could be a breakthrough therapy to address this unmet need.”
The randomized double-blinded, placebo-controlled pivotal study of CyIS was conducted at the University of Pittsburgh School of Medicine. The study began in 1998 and enrolled both single- and double-lung transplant patients who were already on standard, oral immunosuppressive therapies. Enrollment was completed in August 2001, and all subjects were followed until study completion in August 2003. Patients received either CyIS (n=26) or placebo (n=30), in addition to maintenance immunosuppression, and underwent an initial 10-day dose escalation phase to reach a maximum tolerated dose, up to 300 mg. Following initiation, patients received a maintenance dose of either the CyIS or placebo three times per week for two years. Upon completion of dosing, all subjects were followed for efficacy, including chronic rejection and survival, until the last enrolled subject completed the two-year period of dosing.
Analysis of data from the initial study period showed a 79 percent decrease in the risk of death for patients receiving CyIS compared to patients receiving placebo. Data from an additional 10 months of follow-up show that the survival duration for CyIS-treated patients remained significantly higher versus placebo-treated patients (log-rank p=.017). Estimated four-year survival was 84 percent in CyIS-treated subjects compared to 56 percent in placebo-treated subjects. The estimated hazard ratio (CyIS/placebo) of 0.31 corresponds with a 69 percent reduction in mortality.
CyIS therapy delivers cyclosporine directly to the lungs, achieving greater drug concentration at the site of rejection. A New Drug Application (NDA) for CyIS (tradename PULMINIQTM) was submitted to the U.S. Food and Drug Administration (FDA) by Chiron Corporation in October 2004 and is now under review. Cyclosporine in other formulations is a well-established immunosuppressive therapy for kidney, liver and heart transplant recipients. Currently, there are no FDA-approved therapies for the prevention of chronic rejection.
Compared to other organ transplants, long-term survival following lung transplantation has not improved appreciably in the last 10 to 15 years. According to 2004 ISHLT registry data of lung transplants performed between January 1998 and June 2002, one-year survival remains about 75 percent. At five years, survival remains approximately 45 percent, essentially unchanged since the late 1980s and early 1990s, and is significantly lower than survival rates following other solid organ transplants.
About Lung Transplant Rejection
Following transplantation there is an inherent risk of rejection, where the recipient’s immune system will recognize the donated lungs as foreign and attack the transplanted organ. Within the first three months, patients are at highest risk of acute rejection. However, as the patient moves out in time, the primary cause of death in up to 76 percent of cases is chronic rejection, which usually manifests after the first year. This is characterized by chronic inflammation and irreversible scarring of the lungs, a condition known as bronchiolitis obliterans.
Media Contact
More Information:
http://www.ishlt.orgAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
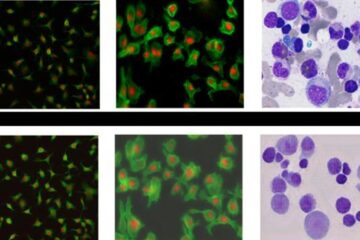
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















