Generation gap found in chronic pain

Younger adults don’t cope as well with pain as their elders, study finds, but blacks feel it worse
Adults under the age of 50 who have chronic pain may be less able to cope with their condition and more prone to associated depression than their elders, a new study suggests. And the same “generation gap” pattern exists among both blacks and whites, though blacks of all ages have previously been found to experience more pain and more pain-related negative effects than whites.
The study also finds that in general, blacks scored higher than whites on measurements of the intensity of their pain, disability related to their pain, and depression symptoms. This finding is consistent with past studies on pain that examined racial differences in chronic pain experience.
The new study, by researchers at the University of Michigan and the University of South Florida, appears in a special issue of the journal Pain Medicine, published by the American Academy of Pain Medicine. The issue focuses on the differences in pain, pain effects and pain treatment that are increasingly being found between members of different racial and ethnic groups. “No matter what your color or age, chronic pain has a major impact on your life and your ability to work or function,” says the study’s senior author, U-M pain specialist Carmen R. Green, M.D., who is co-guest editor of the special issue. “Our study suggests that age is a significant factor across races and ethnicities, and that the impact of pain may differ even within racial and ethnic groups.” Green recently was named an inaugural Mayday Pain and Society fellow by the Mayday Pain Project.
The new study examined detailed data from 5,823 black and white adults treated at the U-M Multidisciplinary Pain Center over eight years. They were divided into two groups: those under age 50, and those over age 50. During their evaluation for pain treatment, the patients completed standardized questionnaires that assessed their mental and physical status, as well as the intensity and impact of their pain, the ability to cope with their pain, sleep and alcohol use patterns, and symptoms of depression and post-traumatic stress disorder that can result from painful medical conditions or an incident that results in chronic and persistent pain. The study was retrospective and cross-sectional, and it included patients with many chronic pain conditions. Within both racial groups, there were significant differences between the age groups.
Older whites, and older blacks, were better able to cope with their pain, had less trouble falling asleep, and had fewer depressive symptoms than younger members of their racial group. Even after the researchers corrected for differences in the number of months the patients had lived with their pain, and for differences in gender, marital status and education, the effects remained.
Why the gap? A combination of generational characteristics and attitudes, life experiences and age-related health expectations may be at play, though more research is needed to find out, say Green and her colleague Tamara Baker, Ph.D., of USF’s School of Aging Studies. Baker formerly was a postdoctoral fellow at the U-M School of Public Health’s Center for Research on Ethnicity, Culture and Health.
“Older people may feel that pain is just something that you deal with, perhaps because they were raised in a time when pain was not addressed in the way we deal with it today, or because they feel that pain is just a normal part of getting older,” says Green, an associate professor of anesthesiology at the U-M Medical School and attending physician at the U-M Center for Interventional Pain Medicine.
“But younger people, who may be dealing with job and family stress in addition to their pain, may experience more negative effects,” she continues. “They may also have different expectations about pain treatment and about experiencing chronic pain at a relatively young age. This is particularly important because the prevalence of chronic pain is increasing.”
Indeed, recent advances in pain diagnosis and treatments, and in the training of doctors and nurses to see pain as a vital sign just like temperature and pulse rate, mean that more patients are getting effective relief for their chronic pain than ever before. So, younger people may just expect more from pain treatment than their elders do.
Green and Baker note that assessing depression symptoms in people being treated for chronic pain is complicated by a sort of “chicken and egg” problem: depression itself can cause or exacerbate vague pain, but it can also be triggered by a stressful event such as an injury or illness that itself causes pain. It is important to note, they say, that when a person has chronic pain, other problems such as depression, anxiety and sleep disturbances often follow.
For blacks, age isn’t the only factor. They are more likely than whites to have several chronic illnesses associated with pain, ranging from diabetes to heart disease and arthritis. They are also more likely to experience increased disability associated with those diseases. Numerous studies have shown that blacks and members of other racial and ethnic minorities are consistently under-treated for pain across a range of conditions, from cancer and chest pain to acutely painful conditions like broken bones and chronic lower-back pain.
And Green’s own previous work has also shown that, regardless of their age, blacks with chronic non-cancer pain from any source suffered more psychological and physical effects than whites. Other research by Green and her colleagues has shown that access to pain care and pain medications can also vary by race and ethnicity. For instance, pharmacies in neighborhoods with large minority populations tend not to carry narcotic pain medicines such as morphine.
Green hopes that the new study, and others in the special issue of Pain Medicine, will continue to draw the attention of pain researchers and plant the seeds for further research in this area. “These findings are particularly important when you consider that pain is estimated to impact more than 100 million Americans, and will clearly impact independence and successful aging,” she says.
Media Contact
More Information:
http://www.umich.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
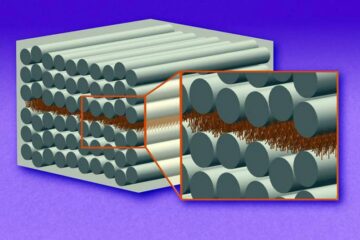
“Nanostitches” enable lighter and tougher composite materials
In research that may lead to next-generation airplanes and spacecraft, MIT engineers used carbon nanotubes to prevent cracking in multilayered composites. To save on fuel and reduce aircraft emissions, engineers…

Trash to treasure
Researchers turn metal waste into catalyst for hydrogen. Scientists have found a way to transform metal waste into a highly efficient catalyst to make hydrogen from water, a discovery that…
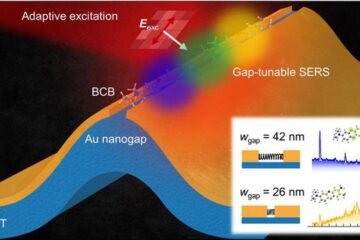
Real-time detection of infectious disease viruses
… by searching for molecular fingerprinting. A research team consisting of Professor Kyoung-Duck Park and Taeyoung Moon and Huitae Joo, PhD candidates, from the Department of Physics at Pohang University…





















