New marrow transplant method developed at Stanford may eliminate fatal side effects

Bone marrow transplantation can cure lymphomas and leukemia, but in about half of the cases transplanted immune cells wind up attacking the patient’s body, as well as the cancer.
In response to this problem, researchers at the Stanford University School of Medicine have developed a technique that can virtually eliminate this life-threatening complication, known as graft-versus-host disease, without compromising the transplanted cells’ effectiveness against cancer.
The therapy entails adjusting the patient’s level of a specific type of immune cell, the regulatory T cells, before the transplant is done. The method was first developed in mice by Samuel Strober, MD, professor of medicine (immunology and rheumatology), who has been studying these types of cells for more than 25 years. Robert Lowsky, MD, assistant professor of medicine (bone marrow transplantation), has adapted this strategy for humans along with Strober, and will present the results of tests Dec. 6 at the annual American Society of Hematology meeting in San Diego.
In two clinical trials funded by the National Institutes of Health, Lowsky, Strober and other colleagues found that only one of the 37 patients who received the treatment developed graft-versus-host disease. “You would have expected something in the order of 30 to 60 percent incidence of severe graft-versus-host disease in these patients, according to conventional methods,” said Strober.
Studies of the new method found there was no increase in the rate of infections in the treated patients. The studies also found that the majority of patients who were in partial remission went into complete remission, and those who were in complete remission didn’t relapse. “It looks like there is a potent anti-tumor effect from our method despite the incidence of graft-versus-host disease being dramatically lowered,” said Lowsky.
Also at the conference, Strober will conduct a session in which he reviews the checkered history of regulatory T cells. For years immunologists were polarized into groups who believed in the cells, once known as suppressor T cells, and those who doubted their existence. But with the development of more advanced techniques for distinguishing between the different types of immune system cells, the existence of the regulatory T cells has been confirmed. The latest research suggests that the regulatory T cells act as the immune system’s peacekeepers, signaling to other T cells when to hold off from attacking an intruder.
“The news going into this meeting is that the field of regulatory T cells has not only come out of the clouded period that it was in, but is now being accepted and adapted into clinical trials as a conceptual framework for achieving certain desirable outcomes, for example in the area of bone marrow transplantation,” said Strober.
Always a proponent of the existence of regulatory T cells, Strober worked out over the years a strategy using irradiation and antibodies to increase the relative amount of regulatory T cells in the immune tissues of host mice from about 1 percent of the total T cells to more than 90 percent. By increasing the relative amount of these cells, he found that he could retain the desired effect of killing cancerous cells following bone marrow transplantation, but eliminate the attack on host tissues. “It allows you to throw out the one effect but not the other,” he said.
Lowsky said he and Strober have now taken Strober’s animal model and translated it to the clinical setting for people. Although they have not yet gathered conclusive evidence that this cellular process worked the same in humans as it did in mice-that would require doing direct examinations of cells from patients’ spleens or lymph nodes-Lowsky said their evaluations of the blood and marrow samples suggest that is the case.
Now that the method is proving to be a viable therapy for humans, the team will be testing it with other cancer centers.
Others involved in the clinical trial are Robert Negrin, MD, professor of medicine; Yinping Liu, MD, a staff research associate and Judith Shizuru, MD, PhD, associate professor of medicine, all in the bone marrow transplantation division, and Tsuyoshi Takahashi, MD, a research fellow in Strober’s lab.
Media Contact
More Information:
http://www.stanford.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
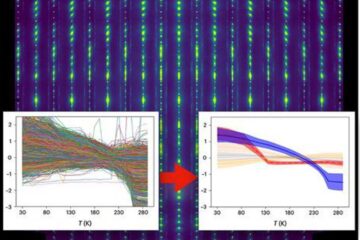
Machine learning algorithm reveals long-theorized glass phase in crystal
Scientists have found evidence of an elusive, glassy phase of matter that emerges when a crystal’s perfect internal pattern is disrupted. X-ray technology and machine learning converge to shed light…
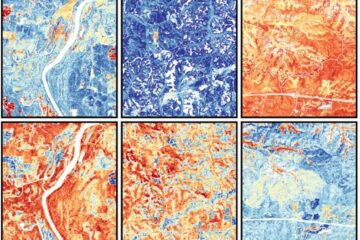
Mapping plant functional diversity from space
HKU ecologists revolutionize ecosystem monitoring with novel field-satellite integration. An international team of researchers, led by Professor Jin WU from the School of Biological Sciences at The University of Hong…

Inverters with constant full load capability
…enable an increase in the performance of electric drives. Overheating components significantly limit the performance of drivetrains in electric vehicles. Inverters in particular are subject to a high thermal load,…





















