Some AIDS Drugs Promote Neurological Damage

One group of drugs that is effective in fighting HIV may, paradoxically, also be promoting the death of sensory nerves in the skin, according to a study presented October 5, 2004, at the 129th annual meeting of the American Neurological Association in Toronto.
A team of American and Australian researchers reported that the use of certain anti-HIV drugs, called dideoxynucleosides, is highly correlated with a condition called sensory neuropathy, in which patients experience constant pain, and abnormal sensations including numbness and sensitivity, in the feet and legs. In a separate presentation, presented on October 4, the same investigators showed that simple punch skin biopsies are an effective way of identifying sensory neuropathy, possibly even before symptoms appear.
Dideoxynucleosides, members of a class of drugs called ’nucleoside reverse transcriptase inhibitors’ are common component of highly active antiretroviral therapy (HAART), the so-called AIDS “cocktails” that prevent HIV from duplicating itself. The authors noted that these drugs are frequently included in the generic HAART combinations used in Africa and India. “Because the introduction of HAART has reduced the rates of HIV-associated dementia and opportunistic infections, sensory neuropathies have become the commonest neurological disorders associated with AIDS,” said lead author Justin C. McArthur, MD, of Johns Hopkins University in Baltimore, Maryland.
The factors that lead to HIV-associated sensory neuropathy are not clear. Diabetes, intravenous drug use, or hepatitis C may contribute to heightened susceptibility, along with some of the same drugs that help protect against HIV.
In the present study, McArthur and his colleagues at Johns Hopkins and at the Alfred Hospital, Burnet Institute, and Monash University in Melbourne, Australia studied the relationship between the use of three dideoxynucleosides called ddC, ddI, and d4T and the occurrence of sensory neuropathy. The researchers combined data from two diverse study populations in Baltimore and Melbourne, with significant (and preplanned) differences in terms of racial demographics and history of IV drug use, male homosexual relations, and hepatitis C co-infection. “We found a strong association between previous or current use of ddC, ddI, or d4T and the presence of symptomatic sensory neuropathy,” said McArthur.
In a separate study in the same subjects, led by medical student Siva P. Raman, McArthur’s team used skin biopsies to determine whether the extent of HIV-sensory neuropathy was associated with a loss of the smallest sensory fibers in the skin, which are responsible for transmitting pain sensations. This method has been proposed as a way to measure the extent of sensory neuropathy and also to detect nerve damage that has not reached the stage where it causes pain or numbness.
Raman, McArthur, and colleagues found that the biopsy method correlates well with the extent of sensory neuropathy, and they were also able to detect nerve abnormalities in a substantial number of HIV patients who had not yet developed sensory neuropathy. They also showed that factors such as hepatitis C co-infection or vitamin B-12 deficiency, among others, were not apparently associated with the loss of small nerve fibers in the skin.
[abstracts]
323. Antiretroviral Exposure Is a Risk Factor for HIV-Associated Sensory Neuropathies, Justin C. McArthur, Jason Creighton, Richard Skolasky, Luxmi Lal, Richard Moore, Steven Wesselingh, and Katherine Cherry; Baltimore, MD and Melbourne, Victoria, Australia
Background: specific reverse transcriptase inhibitors may provoke HIV-associated sensory neuropathies (SN). Methods: 156 HIV+ adults underwent standardized clinical/physiological assessments. PGP9.5 immunostaining quantified epidermal innervation. Antiretroviral exposure was assessed with multivariate analysis.
Results: at JHU, 86% were black, 35% had a history of IDU, and 71% were HepC+. At MU, 95% were white, 92% had a history of MSM, and 11% were HepC+. HgbA1C levels were > 5.8% in 23% at JHU and 12% at MU (p=0.101). 33% were neuropathy-free, 18% had asymptomatic SN, and 49% symptomatic SN. The likelihood of having symptomatic SN was strongly associated with use of ddI (OR=2.6, p=.024), or d4T (OR=5.1, p=.002). Thermal and vibration thresholds were measured with the Case IV device and vibratory QST was relatively insensitive to symptomatic SN. More morphological abnormalities on skin biopsy were noted in SN subjects, but 23% of neuropathy-free had abnormalities. Conclusions: The frequency of SN was high and correlated strongly with anytime exposure to ddI or d4T. Hepatitis C serostatus did NOT modify the prevalence of SN at baseline. Morphological abnormalities were noted in a high proportion of neuropathy-free subjects. Quantitative sensory testing had a low diagnostic efficiency in this cohort. Study supported by NS44807
WIP4. HIV-associated sensory neuropathies: Relationship to epidermal nerve fiber densities
Siva P Raman, J Creighton, R Skolasky, TBN Cherry, R Moore, Carter K, S Wesselingh, C Cherry, JC McArthur. Baltimore, MD, USA, Melbourne, Australia.
Background: Specific nucleoside reverse transcriptase inhibitors (ddI, d4T, and ddC) provoke symptomatic HIV-associated sensory neuropathies (HIV-SN). The relationship of epidermal nerve fiber densities (ENFD) to symptoms of sensory neuropathy, and the modifying role of hepatitis C, Vitamin B12, HgbA1C, and lactate is uncertain.
Methods: 130 HIV-infected adults underwent standardized clinical and physiological assessment: skin biopsies and assays for hepatitis C (HpC), vitamin B12, hemoglobin A1C, and plasma lactate. Results: At baseline, HAART was used in 79% at JHU, and 90% at MU, with ddI and d4T used together in combination in 4% and 15% respectively. ENFD were calculated for 36 JHU subjects at the distal leg and thigh. The distribution of subjects was (JHU): neuropathy-free 30%; asymptomatic SN (asx-SN) 17%; and symptomatic SN (sx-SN) 52%. The average fiber density (distal leg and thigh) for sx-SN was 5.88, 9.38 for the neuropathy-free group, and 7.41 for the asx-SN, with a significant difference between the groups (p=0.01). There was no correlation between ENFD and Vitamin B12, lactate, Hepatitis C serostatus, or Hemoglobin A1C. Conclusions: ENFD are related to the expression of symptomatic SN, but do not appear to be modified by Hepatitis C, vitamin B12, lactate, and hemoglobin A1C, which are not correlated with fiber densities.
Media Contact
More Information:
http://www.aneuroa.orgAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
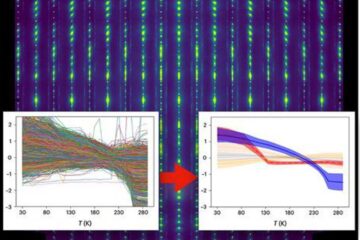
Machine learning algorithm reveals long-theorized glass phase in crystal
Scientists have found evidence of an elusive, glassy phase of matter that emerges when a crystal’s perfect internal pattern is disrupted. X-ray technology and machine learning converge to shed light…
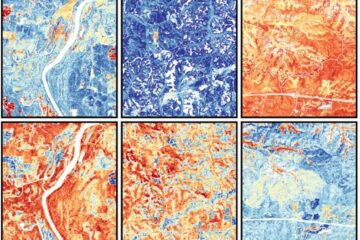
Mapping plant functional diversity from space
HKU ecologists revolutionize ecosystem monitoring with novel field-satellite integration. An international team of researchers, led by Professor Jin WU from the School of Biological Sciences at The University of Hong…

Inverters with constant full load capability
…enable an increase in the performance of electric drives. Overheating components significantly limit the performance of drivetrains in electric vehicles. Inverters in particular are subject to a high thermal load,…





















